When it is functioning normally, you may not give too much thought to the pelvic area of your body or the group of muscles found there known as the pelvic floor. However, the function of your pelvic floor is essential to your ability to control urination, flatulence, and defecation. (4)
Pelvic floor muscle disorders are common, and it’s estimated they will account for 1.6 million medical visits per year by 2030. (2) These disorders, such as pelvic organ prolapse and bowel control problems, can occur when the pelvic floor muscles and connective tissues are damaged or weakened. (7)Pelvic floor physical therapy is a treatment approach for musculoskeletal disorders of the pelvis, intended to improve the strength, endurance, and/or relaxation of the pelvic floor. (4)(10)
What is the pelvic floor?
The term “pelvic floor” describes a group of muscles that form a hammock or dome shape across the bone structure at the bottom of the pelvis. (5)(7) These muscles and their adjoining tissues support the pelvic organs and their functions. (7)The pelvic organs include the:
- Cervix
- Bladder
- Intestines
- Rectum
- Urethra
- Uterus
- Vagina (7)
Pelvic floor muscles
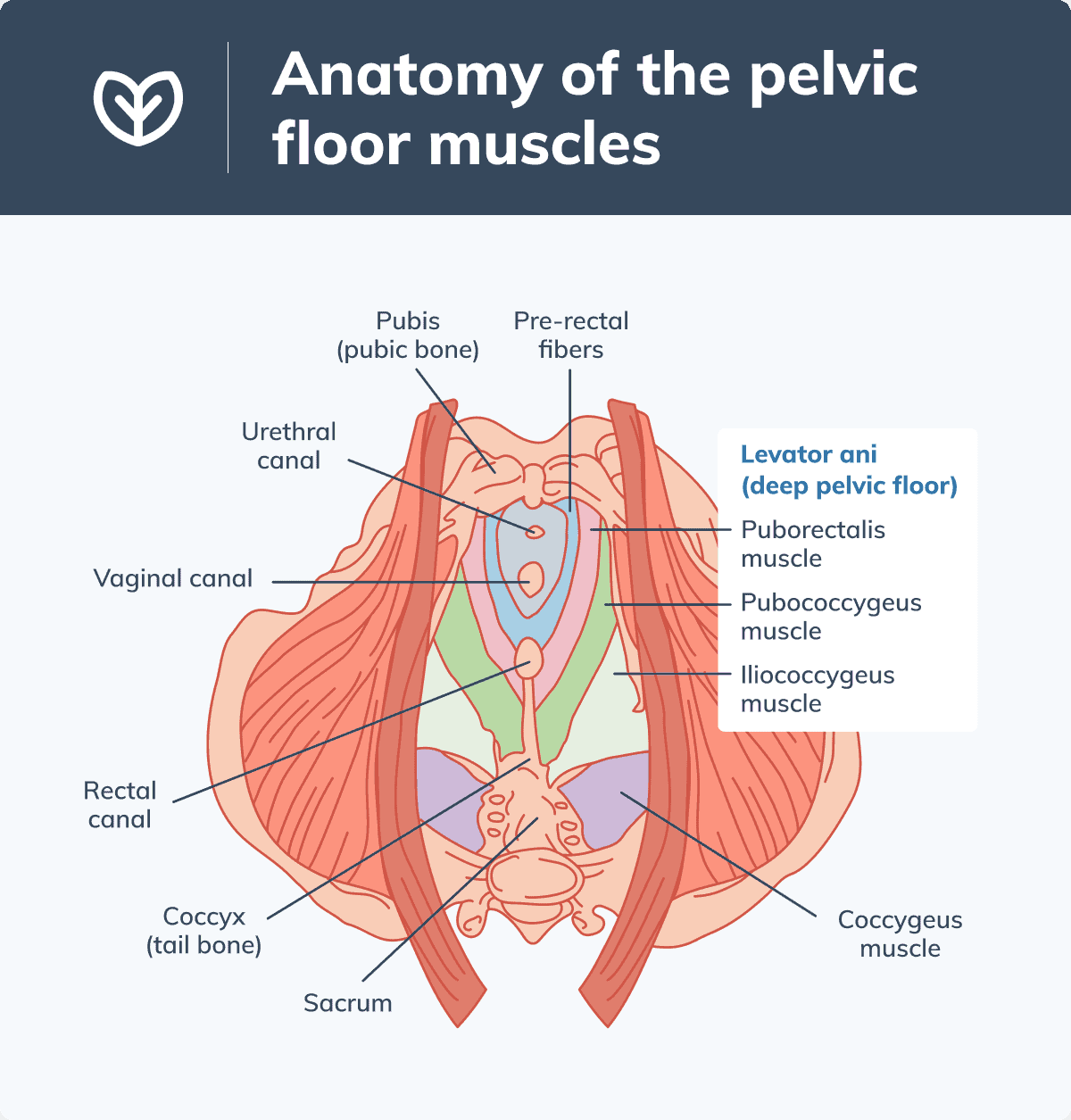
The pelvic floor muscles span from the pubis (pubic bone) at the front of the body to the sacrum and coccyx (tail bone) at the back of the body. (5)The pelvic floor is classified into two groups: the superficial (surface) pelvic floor and the levator ani (deep pelvic floor). The superficial pelvic floor muscles include the bulbocavernosus, ischiocavernosus, and transverse perinei. The deep pelvic floor muscles are the puborectalis, pubococcygeus, and iliococcygeus. (4)
The deep muscles are a substantial part of the pelvic floor volume. The puborectalis wraps around the anorectal junction (lower part of the rectum). The pubococcygeus and the iliococcygeus elevate and support the pelvic organs. The pubococcygeus also creates an opening for the urethra, anus, and in females, the vagina. (5) Another pelvic floor muscle, the coccygeus, is found towards the back of the body. (2)
The pelvic floor is a group of muscles found across the base of the pelvis. (4)
Functions of the pelvic floor
As mentioned, the pelvic floor muscles provide physical support for the pelvic organs, elevating and holding them in place. (7) In addition, with contraction and relaxation, these muscles influence respiration and pelvic organ functions. (2) The pelvic floor muscles contract during sexual activity, specifically orgasm, providing sexual appreciation. (2)(4)The pelvic floor provides stability to the core and supports posture and movement. (2)(4) Along with associated muscles, the pelvic floor is activated when we sit, stand, maintain an upright position, twist, cough, and sneeze. During standing and walking, contractions of the pelvic floor help distribute loads from the upper limbs and torso to the lower limbs, and vice versa. (2)
Understanding pelvic floor dysfunction
Pelvic floor dysfunction can occur when the pelvic muscles and associated connective tissues become weakened or damaged. (7) This dysfunction may lead to a number of pelvic floor disorders.Bladder dysfunction
The inability to control urine, known as urinary incontinence, can occur in both sexes. Symptoms can include urinary leakage and excessive urinary frequency and urgency. Urinary leakage may occur during coughing and sneezing or due to other factors. (7)Bowel control problems
Similarly, all individuals can experience fecal incontinence, which is the inability to control stool. Fecal incontinence involves the leaking of liquid or solid stool from the rectum. (7)Pelvic organ prolapse
When the pelvic floor cannot support one or multiple pelvic organs, individuals can experience pelvic organ prolapse. Pelvic organ prolapse is characterized by pelvic organs dropping or pressing into the vagina. Prolapse can occur with the bladder, rectum, uterus, or top of the vagina. (1)Symptoms of pelvic floor dysfunction
Symptoms of pelvic floor dysfunction vary depending on the affected area of the pelvis. (2) Signs and symptoms may include:- Constipation (7)
- Difficulty inserting tampons (1)
- Difficulty making it to the restroom in time
- Difficulty starting to urinate or emptying the bladder
- Fecal incontinence
- Feeling heaviness, pulling, or pain in the vagina
- Feeling or seeing a bulge come out of the vagina
- Inability to control flatulence
- Increased frequency and/or urgency of urination (7)
- Low back pain (2)
- Pain during urination (7)
- Urinary leakage during coughing, exercising, or laughing (7)
Risks for pelvic floor dysfunction
Causes and risk factors for pelvic floor dysfunction include:- Age: increased risk with aging and menopause (7)
- Childbirth, pregnancy (4)
- Chronic constipation, straining during bowel movements
- Chronic coughing (e.g., from smoking or health conditions)
- Genetics: being born with conditions that affect connective tissue strength (7)
- Gynecologic or urologic surgery/procedures (e.g., hysterectomy, caesarean section) (4)(7)
- Overweight or obesity (2)
- Race: increased risk in Latina and Caucasian women (7)
- Repeated pressure or minor trauma (e.g., dance, gymnastics, heavy lifting) (4)(7)
- Sexual abuse (4)

Physical pressure or damage, due to factors such as pregnancy and childbirth, may impair the pelvic floor muscles. (4)
What is pelvic floor therapy?
Pelvic floor physical therapy is a treatment approach used by physical therapists with additional training in manual therapy techniques. (3) It includes interventions such as biofeedback, which involves training pelvic floor muscles to relax and contract while using electrodes to monitor physiological responses; neuromodulation, which uses medical devices to increase or decrease specific nervous system activity; and myofascial release, a manual therapy that targets myofascial tissue, a type of connective tissue. Additionally, pelvic floor physical therapy includes therapeutic exercises and stretching. (6)Pelvic floor physical therapy can address chronic pelvic pain syndrome, (6) fecal incontinence, and urinary incontinence, such as incontinence after prostatectomy (surgical treatment of prostate cancer). (8) Pelvic floor physical therapy may also improve sexual dysfunction, including erectile, ejaculation, and orgasm dysfunctions. (3)
Pelvic floor therapy is also used to improve pelvic organ prolapse symptoms, urinary or fecal incontinence, and pelvic floor dysfunction during pregnancy or postpartum. Pelvic floor physical therapy may also benefit individuals with hypertonic pelvic floor disorders, characterized by excessive tension of the pelvic floor, such as pelvic floor myofascial pain. (10)
Pelvic floor physical therapy exercises
What does pelvic floor physio involve? A physical therapist may use a number of manual therapy techniques and provide guidance on pelvic floor training exercises. Treatment for pelvic organ prolapse may also include the use of medical devices and surgery. (5)(7)Types of pelvic floor training exercises
The following are exercises commonly used to target the pelvic floor muscles and improve symptoms of pelvic floor dysfunction.Bladder training
Bladder training, intended to help regain bladder control, involves following a set bathroom schedule, and slowly increasing the duration of intervals until using the bathroom every two and a half to three hours. (7)Kegel exercises
Pelvic floor muscle training, commonly referred to as Kegel exercises, involves routinely squeezing and relaxing pelvic floor muscles. Kegel exercises may be used to improve symptoms of prolapse and urinary incontinence, but have not been shown to resolve pelvic organ prolapse. (7)How do you do pelvic floor therapy?
Kegel exercises can be done with the guidance of a physical therapist or on your own. (7) Pelvic floor physical therapy at home can include Kegel exercises, done by contracting the pelvic floor muscles, which are the same muscles you would squeeze to prevent passing urine or gas. Be sure to continue breathing and do not to activate (squeeze) other muscles, such as muscles in the stomach, buttocks, or thigh. (9)In individuals with penises, it is recommended to do Kegel exercises in front of a mirror to observe movement. You should try to move your penis up and down as an isolated movement (without moving the rest of the body). (1)
In individuals with vaginas, Kegel exercises are done by squeezing the muscles that stop the flow of urine, holding, and then relaxing. It’s suggested to squeeze and hold for three seconds, then relax for three seconds for ten rounds, three times per day. Increase the holding time by one second per week until you reach a ten-second hold time. (1)
How do I know if I need pelvic floor therapy?
If you experience symptoms of pelvic floor dysfunction, listed above, we suggest consulting with your integrative healthcare provider, who can assess your symptoms and health state, as well as recommend treatment and refer you to a qualified physical therapist if appropriate.Pelvic floor physical therapy devices
A medical device known as a vaginal pessary may be used in individuals with pelvic organ prolapse to support pelvic organs and improve bladder control. A pessary is inserted into the vagina by the individual or their healthcare provider, who will advise on the appropriate size, use, and care of the device. (1)(7)The bottom line
Pelvic floor physical therapy is used to strengthen, relax, and improve the function of the pelvic floor muscles. (4)(10) This therapeutic approach has been found to improve symptoms of pelvic floor dysfunction, such as urinary incontinence, fecal incontinence, and pelvic organ prolapse. Pelvic floor therapy should be done with the guidance of a qualified integrative healthcare practitioner.- American College of Obstetricians and Gynecologists. (2020, January). Pelvic support problems. ACOG. https://www.acog.org/womens-health/faqs/pelvic-support-problems
- Bordini, B., Sugumar, K., & Leslie, S. W. (2021). Anatomy, abdomen and pelvis, pelvic floor. In StatPearls, Treasure Island. https://www.ncbi.nlm.nih.gov/books/NBK482200/
- Cohen, D., Gonzalez, J., & Goldstein, I. (2016). The role of pelvic floor muscles in male sexual dysfunction and pelvic pain. Sexual Medicine Reviews, 4(1), 53–62.
- Fitzgerald, C. M., & Hynes, C. K. (2009). Female Perineal/Pelvic pain: The rehabilitation approach. Current Therapy in Pain, 227–233.
- Grimes, W. R., & Stratton, M. (2021). Pelvic floor dysfunction. In StatPearls, Treasure Island. https://www.ncbi.nlm.nih.gov/books/NBK559246/
- Masterson, T. A., Masterson, J. M., Azzinaro, J., Manderson, L., Swain, S., & Ramasamy, R. (2017). Comprehensive pelvic floor physical therapy program for men with idiopathic chronic pelvic pain syndrome: A prospective study. Translational Andrology and Urology, 6(5), 910–915.
- National Institute of Child Health and Human Development. (2020, August 1). About pelvic floor disorders (PFDs). https://www.nichd.nih.gov/health/topics/pelvicfloor/conditioninfo
- Strączyńska, A., Weber-Rajek, M., Strojek, K., Piekorz, Z., Styczyńska, H., Goch, A., & Radzimińska, A. (2019). The impact of pelvic floor muscle training on urinary incontinence in men after radical prostatectomy (RP) – A systematic review. Clinical Interventions in Aging, 14, 1997–2005.
- Urology Care Foundation. (n.d.). Pelvic floor muscles: Symptoms, diagnosis & treatment. https://www.urologyhealth.org/urology-a-z/p/pelvic-floor-muscles
- Wallace, S. L., Miller, L. D., & Mishra, K. (2019). Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Current Opinion in Obstetrics & Gynecology, 31(6), 485–493.





