Meniere’s disease diagnosis
Diagnosing Meniere’s disease can be challenging because it is highly individualized with a symptom profile that can vary from one patient to the next. Some patients may experience a single attack of dizziness infrequently, while others may have several sudden attacks of dizziness frequently over several days or attacks so severe that it causes them to lose balance and fall. (10)Symptom assessment is important to establishing a diagnosis, especially when it comes to vertigo, which is a whirling sensation that can cause loss of balance. With Meniere’s disease, dizziness episodes can last from 20 minutes to 12 hours, possibly leading to nausea, vomiting, diarrhea, and sweating. (3) These episodes of vertigo are typically accompanied by sensorineural hearing loss, aural fullness, and tinnitus, and patients may also have comorbidities that include migraine or autoimmune illnesses, such as lupus, psoriasis, or rheumatoid arthritis. (7)

Definitive Meniere’s disease diagnosis is characterized by the following:
- Two or more spontaneous episodes of vertigo, each lasting 20 minutes to 12 hours
- Audiometrically documented low- to medium-frequency sensorineural hearing loss in one ear at least once before, during, or after one of the vertigo episodes
- Fluctuating aural symptoms, including a feeling of fullness, hearing issues, or ringing/roaring in the affected ear
- No other vestibular diagnosis is present (8)
Meniere’s disease causes
According to the National Institutes of Health, the cause of Meniere’s disease is presently unknown, however, genetics and environmental factors likely play a role in its development. (10) Speculation regarding specific causes are debated in the scientific literature and include:- Abnormal fluctuations with inner ear fluid
- Allergy
- Autoimmunity
- Genetic predisposition
- Hormonal mechanisms (8)
Meniere’s disease triggers
Triggers for this condition, which can be varied and extensive, include:- Atmospheric pressure
- Blood pressure changes
- Crowd noise or sharp noises
- Dairy, chocolate, caffeine, or alcohol
- Head position or quick head movements
- Meal timing
- Physical exertion or tension
- Salt intake
- Seasonal or windy weather
- Stress
- Tiredness
- Traveling by car, bus, train, boat, or airplane
- Visual environments such as reading, looking at water or bright lights, or watching TV (5)
Meniere’s disease treatment
Prioritized in the following order, Meniere’s disease treatment focuses on preventing or reducing the severity and frequency of the following symptoms:- Vertigo
- Hearing loss
- Tinnitus
- Aural fullness
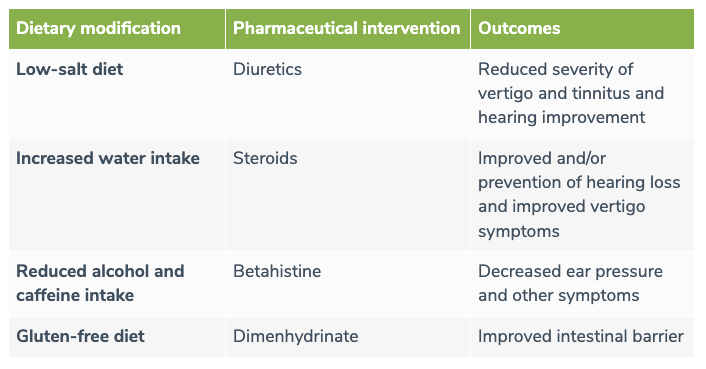
A common conventional medical intervention with Meniere’s disease is the use of diuretics which are believed to reduce fluid in the inner ear; however, in some cases, corticosteroids or betahistine may be prescribed to help with vertigo. (3) The antibiotic gentamicin and surgery are also conventional medical treatment options used to help decrease symptoms of vertigo. (9)
Interventions that can help treat Meniere’s disease included identifying and avoiding the symptom triggers outlined above, as well as achieving relief using specific dietary and lifestyle modifications.

Meniere’s disease lifestyle
Avoiding triggers is a big part of the lifestyle focus but there are other lifestyle factors that can make a difference. Patients with Meniere’s disease often benefit from:- Focusing on both the quantity and quality of sleep each night
- Proactively managing stress
- Sleeping in a dark room to protect circadian rhythm
- Staying well hydrated by drinking fresh water throughout the day (6)
Meniere’s disease diet
Diet can make a big difference when it comes to the quality of life and symptom management for patients diagnosed with Meniere’s disease. The most effective Meniere’s disease diet includes adhering to a low-salt diet, consuming an abundance of water, reducing or avoiding alcohol and caffeine, and following a gluten-free diet. (4)In many cases, specific dietary modifications can result in significant positive effects. (4)
The bottom line
Meniere’s disease can be difficult to diagnose, and because there is no clear cause, treatment can be even more complex. Through an integrative dietary and lifestyle approach, patients with Meniere’s disease can achieve symptom relief and a better quality of life.- Basura, G. J., Adams, M. E., & Monfared A. (2020). Clinical Practice Guideline: Ménière’s Disease Executive Summary. Otolaryngol Head Neck Surg, 162(4), 415-434. https://pubmed.ncbi.nlm.nih.gov/32267820/
- Cunha, F., Settanni, F. A., & Ganança, F. F. (2005). What is the effect of dizziness on the quality of life for patients with Meniere’s disease?. Rev Laryngol Otol Rhinol (Bord), 126(3), 155-158. https://pubmed.ncbi.nlm.nih.gov/16366382/
- Da Cruz, M. (2014). Meniere’s disease: a stepwise approach. Medicine today, 15(3), 18-26. https://medicinetoday.com.au/sites/default/files/cpd/MT2014-03-018-DA%20CRUZ.pdf
- De Luca, P., Cassandro, C., Ralli, M., Gioacchini, F. M., Turchetta, R., Orlando, M. P., Iaccarino, I., Cavaliere, M., Cassandro, E., & Scarpa, A. (2020). Dietary Restriction for The Treatment of Meniere’s Disease. Translational medicine @ UniSa, 22, 5–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7265917/#b12-tm-22-005
- Kirby, S. E., & Yardley, L. (2012). Physical and Psychological Triggers for Attacks in Meniere’s Disease: The Patient Perspective. Psychother Psychosom, 81, 396-398. https://www.karger.com/Article/Fulltext/337114
- Kitahara, T., Okamoto, H., Fukushima, M., Sakagami, M., Ito, T., Yamashita, A., Ota, I., & Yamanaka, T. (2016). A Two-Year Randomized Trial of Interventions to Decrease Stress Hormone Vasopressin Production in Patients with Meniere’s Disease-A Pilot Study. PloS one, 11(6), e0158309. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4928871/
- Magnan, J., Özgirgin, O. N., Trabalzini, F., Lacour, M., Escamez, A. L., Magnusson, M., Güneri, E. A., Guyot, J. P., Nuti, D., & Mandalà, M. (2018). European Position Statement on Diagnosis, and Treatment of Meniere’s Disease. The journal of international advanced otology, 14(2), 317–321. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6354459/
- Oberman, B. S., Patel, V. A., Cureoglu, S., & Isildak, H. (2017). The aetiopathologies of Ménière’s disease: a contemporary review. L’eziopatogenesi della Sindrome di Ménière: stato dell’arte. Acta otorhinolaryngologica Italica : organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale, 37(4), 250–263. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5584095/#!po=3.75000
- Shah, S., Ignatius, A., & Ahsan, S. (2016). It is 2015: what are the best diagnostic and treatments for Meniere’s disease? World Journal of Otorhinolaryngology, 6(1), 1-12. https://www.wjgnet.com/2218-6247/full/v6/i1/1.htm
- US National Library of Medicine. (2020, August). MedlinePlus Meniere’s Disease. https://medlineplus.gov/menieresdisease.html
- Vassiliou, A., Vlastarakos, P. V., Maragoudakis, P., Candiloros, D., & Nikolopoulos, T. P. (2011). Meniere’s disease: Still a mystery disease with difficult differential diagnosis. Annals of Indian Academy of Neurology, 14(1), 12–18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3098516/
- Wu, V., Sykes, E. A., Beyea, M. M., Simpson, M., & Beyea, J. A. (2019). Approach to Ménière disease management. Canadian family physician Medecin de famille canadien, 65(7), 463–467. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6738466/