
What is chronic pain?
Pain is a normal nervous system reaction, alerting individuals that there may be something wrong in the body. (16) Types of pain include inflammatory, musculoskeletal, neuropathic, nociceptive (from physical injury) and psychogenic (from psychological factors). (4) In some cases, acute pain persists and may develop into chronic pain. (17)
Chronic pain is defined as pain persisting longer than 12 weeks, which is generally considered to be a normal tissue healing time. (6)(9) Injury or disease of the nervous system or other body tissues may trigger nervous system sensitization, a factor associated with chronic pain. Other factors that have been identified as playing a role in chronic pain include brain perception and psychosocial factors. (2) The gut microbiota and the metabolites they release, which have been shown to regulate the peripheral and central nervous systems, may also be involved in pain modulation. (8)
What causes chronic pain?
Certain factors may increase an individual’s risk of developing chronic pain, including:
- Advanced age (9)
- Certain health conditions (e.g., anxiety, depression, insomnia, (9) type 2 diabetes, cardiovascular disease) (2)
- Certain nutrient deficiencies (e.g., vitamin D)
- Comorbid (co-existing) chronic diseases
- Environmental factors (e.g., cold climate, lack of sunshine)
- Existing acute or chronic pain within the body
- Female gender
- Genetics: specific genetic variants or a combination of multiple genetic variants
- Interpersonal history (e.g., early life stress or trauma)
- Obesity
- Occupational factors (e.g., work stress, manual labor, unemployment) (9)
- Physical inactivity (2)
- Smoking
- Socio-economic factors (e.g., low levels of education, perceived income inequalities) (9)
- Surgery (7)
Individuals with chronic pain commonly use alcohol, known for its analgesic effects, to treat their symptoms. However, excessive alcohol intake often results in resistance to the analgesic effect. Alcohol withdrawal has been associated with increased pain sensitivity. These factors may promote a cyclical use of alcohol as a way to mask symptoms. (9)
Chronic pain is a common symptom in several health conditions, including:
- Fibromyalgia
- Headache
- Irritable bowel syndrome (IBS) (10)
- Multiple sclerosis (MS) (15)
- Osteoarthritis
- Rheumatoid arthritis (10)

Complications of chronic pain
Individuals with chronic pain may experience a decreased quality of life, as well as an increased risk of suicide and health conditions such as anxiety, depression, and substance abuse. (4) Additionally, pain management and disability associated with chronic pain place a strain on the healthcare system and increase societal costs. (5)(6)Did you know? Individuals with severe pain were found to have more disability and use more health care than those with less severe pain. (11)
Natural pain management approaches
Effective chronic pain treatment involves determining the injury or disease process(es) which are contributing to the pain. (4) Current standard interventions for chronic pain, such as opioids and surgery, may not be beneficial long-term (5) and may be associated with risks, such as overdose-related deaths. (7) An integrative approach to chronic pain may include conventional treatments, as well as diet, dietary supplements, chiropractic care, physical activity, and breathing exercises for pain management. Additional therapies being explored include medicinal cannabis therapy, which has demonstrated some promising results in managing pain in individuals with multiple sclerosis. (15)Best diet for pain management
Researchers have indicated that certain dietary components may reduce pain as a result of managing inflammation and oxidative stress. For example, certain phenolic compounds found in extra virgin olive oil (EVOO), such as lignans and oleuropein, are associated with its anti-inflammatory properties. (13) An anti-inflammatory diet that includes a number of these components may prevent chronic conditions associated with pain. Additionally, the elimination of nightshades and gluten from the diet may help alleviate chronic pain conditions. (17)Dietary supplements
Results from a systematic review identified the dietary supplement types with the most consistent results for reducing pain severity or intensity in individuals with chronic pain. It found that amino acid supplementation, including collagen, carnitine, and theramine, most often demonstrated significant pain reduction results. (2) Clinical trials have highlighted other dietary supplement ingredients that may improve pain, including omega-3 fatty acids, which may be particularly effective in chronic pain associated with dysmenorrhea (menstrual cramps) (12) and vitamin D. (18)Chiropractic treatment
Manual therapies for chronic pain include chiropractic medicine, a licensed healthcare profession focused on the prevention and treatment of neuromusculoskeletal disorders. (14) A systematic review and meta-analysis examined the association between chiropractic treatment and opioid prescriptions in patients with spinal pain, including back and neck pain. In the included studies, the prevalence of individuals who were receiving chiropractic care ranged from approximately 11 to 53%. The study results suggest that individuals with spinal pain undergoing chiropractic care have 64% lower odds of receiving a prescription for opioids than individuals without chiropractic care. (3) These findings indicate that manual therapies such as chiropractic care may be an effective complementary treatment for chronic pain.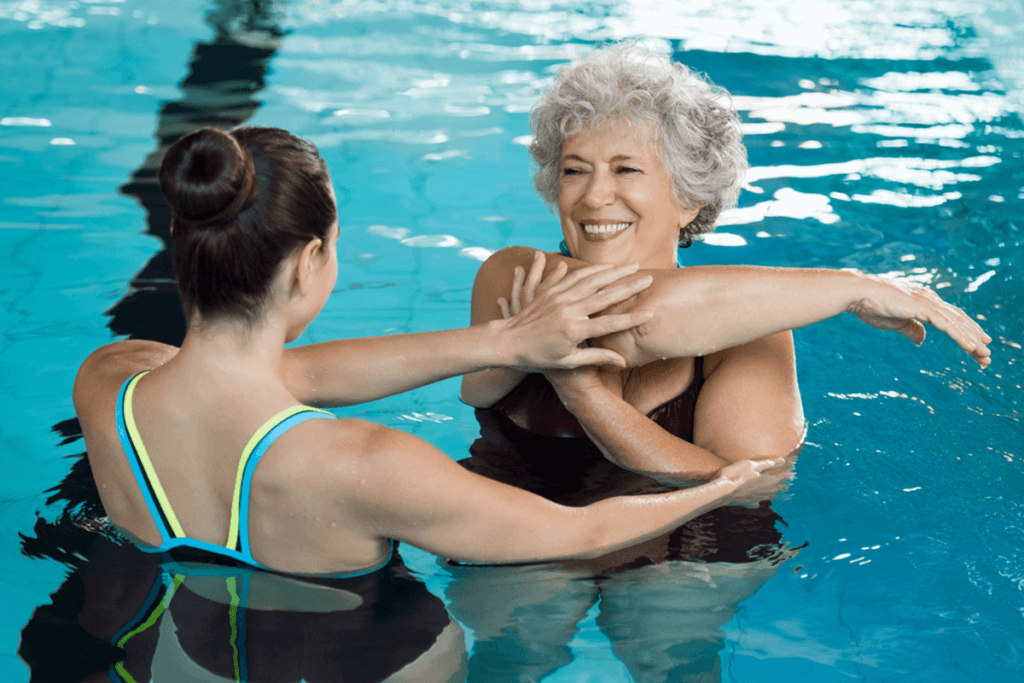
Exercise and pain management
Physical activity has been associated with improvements in individuals with chronic pain, such as reduced pain severity and improved physical function and quality of life. (9) During and following exercise, the body releases various compounds that modulate pain perception, including anti-inflammatory cytokines, endocannabinoids, serotonin, and endogenous opioids (produced within the body). (17) Additionally, exercise may benefit individuals with joint pain as weight loss results in reduced pressure on joints. (6)
Some scientific evidence indicates that certain types of activity may benefit individuals with various chronic pain conditions, including:
- Aquatic exercise, which has been shown to improve chronic back pain
- Supervised aerobic exercise and strength training, which have been shown to reduce pain in individuals with fibromyalgia
- Tai chi, which may reduce arthritic pain (9)
- Yoga, which may improve mental health symptoms in individuals with chronic pain (e.g., anxiety, low mood) (17)
Compliance to any selected exercise regime may be essential to seeing improvement. A greater reduction in pain has been seen in individuals with higher exercise compliance rates than in individuals with uncertain or unmonitored compliance. (9)
Read our tips to stay on track with health and wellness goals on the Fullscript blog.
Breathing exercises for pain management
Researchers suggest that breathing exercises may improve chronic, nonspecific low back pain. The breathing exercise interventions included in one review study ranged from two or three times per week to daily, with durations from four to eight weeks. The study found that breathing exercises were associated with reduced back pain, improved lung function, and increased quality of life. (1)
Final considerations
Chronic pain is a complex symptom implicated in various health conditions. Fortunately, certain natural pain relief interventions may benefit individuals with chronic pain with few adverse effects. (6) If you suffer from chronic pain, consult with your integrative healthcare practitioner to determine which natural pain management approaches are best for your wellness plan.
- Anderson, B. E., & Bliven, K. C. H. (2017). The use of breathing exercises in the treatment of chronic, nonspecific low back pain. Journal of Sport Rehabilitation, 26(5), 452–458.
- Brain, K., Burrows, T. L., Rollo, M. E., Chai, L. K., Clarke, E. D., Hayes, C., … Collins, C. E. (2018). A systematic review and meta-analysis of nutrition interventions for chronic noncancer pain. Journal of Human Nutrition and Dietetics, 32(2), 198–225.
- Corcoran, K. L., Bastian, L. A., Gunderson, C. G., Steffens, C., Brackett, A., & Lisi, A. J. (2019). Association between chiropractic use and opioid receipt among patients with spinal pain: A systematic review and meta-analysis. Pain Medicine, 21(2), e139–e145. https://doi.org/10.1093/pm/pnz219
- Dydyk, A. M., & Conermann, T. (2020). Pain, chronic. In StatPearls . Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK553030/
- Gatchel, R. J., McGeary, D. D., McGeary, C. A., & Lippe, B. (2014). Interdisciplinary chronic pain management: Past, present, and future. American Psychologist, 69(2), 119–130.
- Geneen, L. J., Moore, R. A., Clarke, C., Martin, D., Colvin, L. A., & Smith, B. H. (2017). Physical activity and exercise for chronic pain in adults: An overview of Cochrane reviews. Cochrane Database of Systematic Reviews, 2017(1).
- Glare, P., Aubrey, K. R., & Myles, P. S. (2019). Transition from acute to chronic pain after surgery. The Lancet, 393(10180), 1537–1546.
- Guo, R., Chen, L.-H., Xing, C., & Liu, T. (2019). Pain regulation by gut microbiota: Molecular mechanisms and therapeutic potential. British Journal of Anaesthesia, 123(5), 637–654.
- Mills, S. E. E., Nicolson, K. P., & Smith, B. H. (2019). Chronic pain: A review of its epidemiology and associated factors in population-based studies. British Journal of Anaesthesia, 123(2), e273–e283.
- National Center for Complementary and Integrative Health. (2018, March 27). Complementary health approaches for chronic pain. Retrieved from https://nccih.nih.gov/health/providers/digest/chronic-pain-science
- National Center for Complementary and Integrative Health. (2018b, December 17). Chronic pain: In depth. Retrieved from https://nccih.nih.gov/health/pain/chronic.htm
- Prego-Dominguez, J., Hadrya, F., & Takkouche, B. (2016). Polyunsaturated fatty acids and chronic pain: A systematic review and meta-analysis. Pain Physician, 19(8), 521–535.
- Rondanelli, M., Faliva, M. A., Miccono, A., Naso, M., Nichetti, M., Riva, A., … Perna, S. (2018). Food pyramid for subjects with chronic pain: Foods and dietary constituents as anti-inflammatory and antioxidant agents. Nutrition Research Reviews, 31(1), 131–151.
- Salehi, A., Hashemi, N., Imanieh, M. H., & Saber, M. (2015). Chiropractic: is it efficient in treatment of diseases? Review of systematic reviews. International Journal of Community Based Nursing and Midwifery, 3(4), 244–254.
- Urits, I., Adamian, L., Fiocchi, J., Hoyt, D., Ernst, C., Kaye, A. D., & Viswanath, O. (2019). Advances in the understanding and management of chronic pain in multiple sclerosis: A comprehensive review. Current Pain and Headache Reports, 23(8).
- U.S. National Library of Medicine. (n.d.). Chronic pain. Retrieved February 28, 2020, from https://medlineplus.gov/chronicpain.html
- Yang, S., & Chang, M. C. (2019). Chronic Pain: Structural and functional changes in brain structures and associated negative affective states. International Journal of Molecular Sciences, 20(13), 3130.
- Yong, W. C., Sanguankeo, A., & Upala, S. (2017). Effect of vitamin D supplementation in chronic widespread pain: A systematic review and meta-analysis. Clinical Rheumatology, 36(12), 2825–2833.





