
Breastfeeding offers many benefits to both mom and baby.
Breastfeeding benefits
The American College of Obstetricians and Gynecologists recommends exclusively breastfeeding infants during their first six months of life. After six months, parents are advised to continue breastfeeding with the addition of complementary foods for at least the first year. (1) Besides offering essential nutrition to your growing infant, breast milk confers many other benefits for both mom and baby. The benefits of breastfeeding for infants include:- Improves self-regulation of milk intake compared to formula-fed infants
- Promotes a healthy gut microbiome
- Reduces asthma and allergy rates in breastfed children
- Reduces obesity rates in breastfed children
- Reduces risk of gastrointestinal tract and respiratory tract infections (10)
- Enhances mother-infant bonding
- Decreases visceral fat (excess weight around the midsection)
- Promotes faster postpartum weight loss
- Reduces bleeding post-delivery
- Reduces cardiovascular disease and type 2 diabetes risk
- Reduces breast and ovarian cancer risk (10)
Did you know? In the United States, most mothers try breastfeeding; however, more than half of those women stop breastfeeding earlier than they’d like. (1)
Breastfeeding diet considerations
Breastfeeding mothers require additional nutrition to help support infant growth and development. In addition to eating more calories and macronutrients, your body also has increased demands for many micronutrients.Calories
Breastfeeding mothers require more calories to meet their nutritional needs than non-breastfeeding women. For the average breastfeeding mother, an additional 450 to 500 calories per day is recommended. That works out to be about 2,300 to 2,500 calories per day compared to 1,800 to 2,000 calories per day for a moderately active non-pregnant, non-breastfeeding person. (6) These recommendations may vary depending on your age, activity level, body weight, and extent of breastfeeding. (6) For a personalized calorie recommendation, consult your integrative healthcare provider or refer to the U.S. Department of Agriculture (USDA) My Plate calculator.Macronutrients
As your calorie needs increase, naturally, your macronutrient (i.e., carbohydrate, protein, and fat) requirements will increase as well.Carbohydrate
Consume approximately 45 to 65% of your calories from carbohydrates per day. For example, if you consume 2,400 calories, 270 to 390 g should come from carbohydrate sources. Choose healthy carbohydrate foods such as fruits, vegetables, beans and legumes, whole grains (e.g., quinoa, brown rice, barley), and dairy products. (15)Protein
Aim for 1.1 g of protein per kilogram of body weight per day, which on average may be approximately 71 g per day of protein while nursing. (15)(19) Opt for a combination of plant-based protein sources (e.g., beans, legumes, nuts, seeds) and animal-based protein (e.g., eggs, dairy, lean meat, poultry, fish).Fat
Your fat requirements remain the same pre- and post-pregnancy (20 to 35% of daily calories); however, you’ll typically consume more fat during pregnancy and while breastfeeding simply because you’re eating more total calories. (15) For example, if you consume 2,400 calories per day, you should be eating approximately 53 to 93 g of fat per day. Choose healthy fat sources such as nuts, seeds, avocados, olive oil, and moderate amounts of fish, and limit your intake of processed vegetable oils and fatty cuts of meat. (20)
Focus on consuming a variety of healthy foods, such as vegetables, whole grains, and lean proteins, while you’re breastfeeding and beyond!
Micronutrients
Similar to all life stages, breastfeeding mothers should consume a healthy, well-balanced diet that’s rich in an assortment of fruits, vegetables, whole grains, beans and legumes, nuts and seeds, dairy, and lean animal proteins to help meet their Recommended Dietary Allowances (RDA) of nutrients. That being said, there are some nutrient requirements for breastfeeding moms that exceed the RDA for pregnant and non-pregnant women. These nutrients, along with their common dietary sources, are outlined in the table below.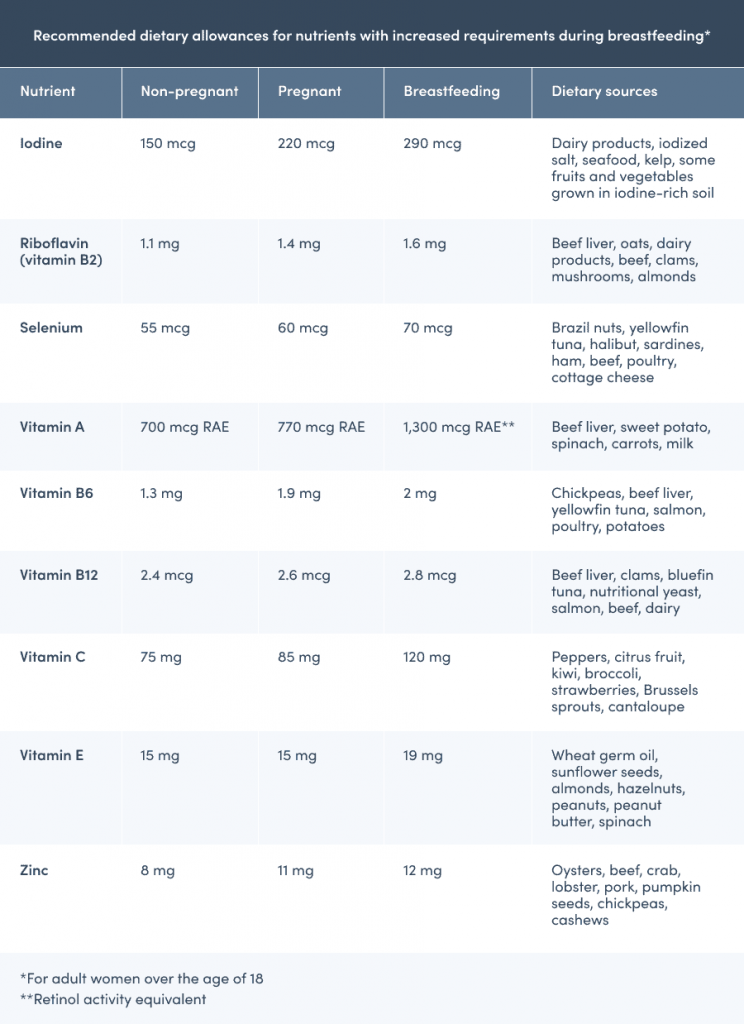
Breastfeeding moms have additional nutrient requirements. The references for this table can be found in the references section below.
Did you know? To help you meet your increased nutrient demands postpartum, your practitioner may recommend that you continue taking your prenatal supplement as you did during pregnancy. You may also be advised to take additional supplementation of certain nutrients if your provider identifies any nutrient deficiencies. (15)
Boosting milk supply: what are galactogogues?
Galactogogues are foods, supplements, or drugs that are believed to increase milk production. (12) Although research is limited, some anecdotal evidence proposes that certain foods are effective galactogogues. Examples of foods that are believed to improve milk supply include: Additional anecdotal evidence suggests that certain supplement ingredients such as fenugreek, blessed thistle, and milk thistle may also support milk production; however, efficacy and safety data is limited. (12) If you’re struggling with your milk supply, consult your integrative healthcare provider before introducing new supplements to your wellness plan.What to avoid or limit while breastfeeding
Certain substances can be passed from the mother to her infant through breast milk, which can be potentially harmful to the infant. For this reason, it’s best to avoid or limit your consumption of the following substances while you’re nursing.Caffeine
Research indicates that it’s safe to consume low to moderate amounts of caffeine per day (≤300 mg or two to three cups of coffee) while breastfeeding. However, high amounts of caffeine (e.g., ten or more cups of coffee) have been shown to cause undesirable side effects in infants, such as irritability, poor sleep, and fussiness. Some mothers and infants may process caffeine more or less efficiently. If you notice any of the previously mentioned signs in your infant shortly after consuming caffeine and nursing, try reducing your caffeine intake. Keep in mind that caffeine can be found in many beverages and some foods, including coffee, energy drinks, tea, and dark chocolate. (6)Alcohol
Although avoiding alcohol entirely while breastfeeding is the safest option, moderate alcohol consumption, defined as no more than one standard drink per day, has not been shown to be harmful to breastfeeding infants. Breast milk contains the highest amount of alcohol approximately 30 to 60 minutes after consumption, and alcohol can often still be detected in breast milk after two to three hours. If you drink alcohol, it’s best to wait a minimum of two hours before nursing. (7) Drinking more than one alcoholic beverage can potentially affect the infant’s growth and development, as well as impair your judgment, making it more challenging and unsafe to care for your baby. (7)Tobacco
Cigarettes, cigars, and other tobacco products contain nicotine and other chemicals that can have harmful effects on your baby. Infants of mothers who smoke have an increased risk for sudden infant death syndrome (SIDS), ear infections, and lower respiratory illnesses. Even babies who aren’t breastfed can suffer these negative health consequences due to exposure to secondhand smoke. (8)Marijuana and CBD
Breastfeeding mothers are generally advised to avoid using marijuana and cannabidiol (CBD) products while breastfeeding. Although data is limited, some research suggests that the chemicals found in marijuana can negatively affect infant brain and motor development. (9) Additionally, the main compound found in marijuana, tetrahydrocannabinol (THC), is stored in the brain and fat tissue and can be slowly released for weeks to months following initial exposure. (13)High-mercury fish
The mercury found in many fish can pass through the mother’s breast milk to the baby and negatively impact their brain and nervous system development. Fish can be safely consumed while breastfeeding; however, it’s important to take some extra precautions to ensure you’re consuming safe options. As a general rule, breastfeeding mothers should avoid high-mercury fish, including shark, swordfish, tilefish, and king mackerel. (15) You can safely enjoy two to three four-ounce servings per week of many types of fish, including anchovies, salmon, catfish, tilapia, and trout. (5)Additional breastfeeding tips
Besides minding your nutritional needs, it’s also essential to support your mental and physical well-being during pregnancy and while breastfeeding.Manage your stress levels
It may be easier said than done, but keeping stress at bay can help improve your milk supply. Research demonstrates that chronic stress and anxiety suppresses milk production by inhibiting the milk-ejection reflex. (14)Stay hydrated
Although drinking more water doesn’t increase milk production, it’s important to drink plenty of water while nursing to compensate for lost fluid. Try to drink a glass of water with meals and each time you nurse. (17)Be active
Research has demonstrated that exercise doesn’t negatively affect milk supply or infant growth. (14) If you feel comfortable and you’ve been given permission by your practitioner, engaging in regular exercise can improve your overall well-being. (18) As long as you had a complication-free vaginal delivery and you’ve been cleared by your practitioner, you can begin to slowly increase the duration and intensity of your physical activity. However, if you delivered your baby via cesarean section or you experienced complications, it’s best to wait until you’re fully healed and you’ve been given permission by your provider. (2)
Improve your mental and physical well-being by making time for moderate physical activity.
Where to seek breastfeeding support
If you’re experiencing difficulties with nursing your infant, you’re not alone. There are many common struggles mothers may encounter, including issues with latching, pain, mastitis, or low milk supply, to name a few. When seeking help, consider the following:- Ask your healthcare provider or pediatrician for support group suggestions.
- Contact the hospital or birthing center where your child was born to see if they have any International Board Certified Lactation Consultants (IBCLC), doulas, or other lactation professionals on staff who lead classes or offer home visits.
- Contact your local Women, Infants, and Children (WIC) office if you’re located in the United States.
- Find a local La Leche League leader or group.
- Receive breastfeeding support and education from the Breastfeeding Committee for Canada and the Canada Prenatal Nutrition Program if you’re located in Canada.
The bottom line
Breastfeeding requires a significant amount of energy and increased nutrient demands. Even after pregnancy, it’s essential to prioritize a healthy, nutrient-dense diet for both you and your baby. If you’re a breastfeeding mother, consult your integrative healthcare provider or lactation professional for breastfeeding tips and recommendations.- ACOG Committee Opinion No. 756. (2018). Optimizing support for breastfeeding as part of obstetric practice. Obstetrics & Gynecology, 132(4), e187–e196.
- American College of Obstetricians and Gynecologists. (2019). Exercise after pregnancy.
- Bazzano, A. N., Cenac, L., Brandt, A., Barnett, J., Thibeau, S., & Theall, K. P. (2017). Maternal experiences with and sources of information on galactagogues to support lactation: A cross-sectional study. International Journal of Women’s Health, Volume 9, 105–113.
- Budzynska, K., Gardner, Z. E., Dugoua, J. J., Low Dog, T., & Gardiner, P. (2012). Systematic review of breastfeeding and herbs. Breastfeeding Medicine, 7(6), 489–503.
- Centers for Disease Control and Prevention. (2019, August 27). Mercury exposure and breastfeeding. https://www.cdc.gov/breastfeeding-special-circumstances/hcp/exposures/mercury.html
- Centers for Disease Control and Prevention. (2021a, January 28). Diet considerations for breastfeeding mothers. https://www.cdc.gov/breastfeeding-special-circumstances/hcp/diet-micronutrients/maternal-diet.html
- Centers for Disease Control and Prevention. (2021b, February 9). Alcohol and breastfeeding. https://www.cdc.gov/breastfeeding-special-circumstances/hcp/vaccine-medication-drugs/index.html
- Centers for Disease Control and Prevention. (2021c, February 16). Tobacco, E-Cigarettes and breastfeeding. https://www.cdc.gov/breastfeeding-special-circumstances/hcp/vaccine-medication-drugs/tobacco.html
- Centers for Disease Control and Prevention. (2021d, August 10). Marijuana and breastfeeding. https://www.cdc.gov/breastfeeding-special-circumstances/hcp/vaccine-medication-drugs/marijuana.html
- Dieterich, C. M., Felice, J. P., O’Sullivan, E., & Rasmussen, K. M. (2013). Breastfeeding and health outcomes for the Mother-Infant dyad. Pediatric Clinics of North America, 60(1), 31–48.
- Foong, S. C., Tan, M. L., Foong, W. C., Marasco, L. A., Ho, J. J., & Ong, J. H. (2020). Oral galactagogues (natural therapies or drugs) for increasing breast milk production in mothers of non-hospitalised term infants. Cochrane Database of Systematic Reviews, 5(5), CD011505.
- Forinash, A. B., Yancey, A. M., Barnes, K. N., & Myles, T. D. (2012). The use of galactogogues in the breastfeeding mother. Annals of Pharmacotherapy, 46(10), 1392–1404.
- Garry, A., Rigourd, V., Amirouche, A., Fauroux, V., Aubry, S., & Serreau, R. (2009). Cannabis and breastfeeding. Journal of Toxicology, 2009, 1–5.
- Institute of Medicine (US) Committee on Nutritional Status During Pregnancy and Lactation. (1991) Nutrition During Lactation. Washington (DC): National Academies Press (US); 5, Milk Volume.
- Kominiarek, M. A., & Rajan, P. (2016). Nutrition recommendations in pregnancy and lactation. Medical Clinics of North America, 100(6), 1199–1215.
- Modepeng, T., Pavadhgul, P., Bumrungpert, A., & Kitipichai, W. (2021). The effects of date fruit consumption on breast milk quantity and nutritional status of infants. Breastfeeding Medicine. Published.
- Montgomery, K. S. (2002). Nutrition column: An update on water needs during pregnancy and beyond. The Journal of Perinatal Education, 11(3), 40–42.
- Norman, E., Sherburn, M., Osborne, R. H., & Galea, M. P. (2010). An exercise and education program improves Well-Being of new mothers: A randomized controlled trial. Physical Therapy, 90(3), 348–355.
- U.S. Food and Drug Administration. (2016). Frequently asked questions for industry on nutrition facts labeling requirements. https://www.fda.gov/media/99069/download
- U.S. National Library of Medicine. (2015). Dietary fats. https://medlineplus.gov/dietaryfats.html





