ADHD symptoms
Characteristics of ADHD include patterns of inattention and/or hyperactivity and impulsivity that are severe, persistent, and interfere with functioning or development. (18)(22) While most children display both inattention and hyperactivity/impulsivity, two subgroups of ADHD have been identified based on which behavior is more pervasive: primarily inattentive and primarily hyperactive-impulsive. (14)(22) ADHD diagnosis typically occurs in children between the ages of three and six, and its symptoms may also persist throughout adolescence and adulthood, although often less severe. (23)
- Inattention to detail, careless mistakes
- Difficulty listening and paying attention
- Difficulty following instructions and meeting deadlines
- Poor time management
- Poor organization of tasks and belongings
- Forgetful, often lose things
- Easily distracted
- Difficulty sitting still, fidgeting, squirming
- Restlessness
- Running around or climbing in inappropriate situations
- Inability to play or engage in activities quietly
- Talking incessantly
- Interrupting frequently, blurting out answers, finishing others’ sentences
- Speaking or acting out of turn (22)
What causes ADHD?
While the causes of ADHD in children remain unclear, a combination of genetic and environmental factors are believed to play a role in the development of the condition, including:- Very low birth weight, lack of oxygen at birth
- Exposure to alcohol, cigarette smoke, or drugs during pregnancy (14)(22)
- Exposure to environmental toxins during pregnancy and/or at a young age Brain injury
- Gender (more common in males) (22)
How to treat ADHD: diet, supplementation, and lifestyle
ADHD is typically addressed using medication (e.g., stimulants), psychotherapy, behavioral therapy, or a combination. (22) According to the 2016 Centers for Disease Control and Prevention study, 62% of children diagnosed with ADHD were taking medication and 47% had received behavioral therapy in the past year. (6) However, researchers recommend a multimodal approach to pediatric ADHD treatment. (18)Did you know? According to a 2015 study examining the use of nutritional supplements in the treatment of ADHD, 12–64% of children use some form of complementary medicine to address their condition. (4)The information below provides an overview of the roles of diet, supplementation, physical activity, and sleep in the treatment of ADHD.

Diet and ADHD
In the 1970s, the Feingold diet was the first proposed dietary intervention for ADHD. Based on the belief that ADHD symptoms in kids were caused by food additives, the diet involved omitting a number of foods from the diet, including apples, grapes, processed meats, and any foods with artificial flavoring, coloring, and preservatives. While there is mixed evidence on the effectiveness of the Feingold diet, recent versions of the diet now recommend only the exclusion of artificial coloring and other additives. (18) Current research on ADHD suggests that food additives may be implicated in a subgroup of ADHD cases. (27)(36) A 2012 meta-analysis reported that synthetic food coloring may be related to symptoms and signs of ADHD in approximately 8% of children with the condition. Unfortunately, research in this area is often conducted with small sample sizes and prone to publication bias. (27) Several studies have also examined the link between ADHD and food intolerances, allergies, or both. In a subgroup of children, an elimination diet may be a valuable method to uncover potential dietary triggers involved in the manifestation of ADHD. (26)(28)(29)Did you know? The elimination diet involves temporarily restricting the intake of potential dietary triggers, such as dairy, wheat, eggs, nuts, and chocolate.The second stage of the diet involves reintroducing potential triggers, one at a time, and monitoring for changes in behavior and symptoms. (18) Visit the Fullscript blog to learn more about the elimination diet.
Nutrients and supplementation for ADHD
While the elimination diet may help determine a relationship between certain foods and symptoms of ADHD, research has also identified a number of nutrients and botanicals that may be beneficial in addressing the symptoms of ADHD. The following table provides examples of these supplemental nutrients and supporting evidence.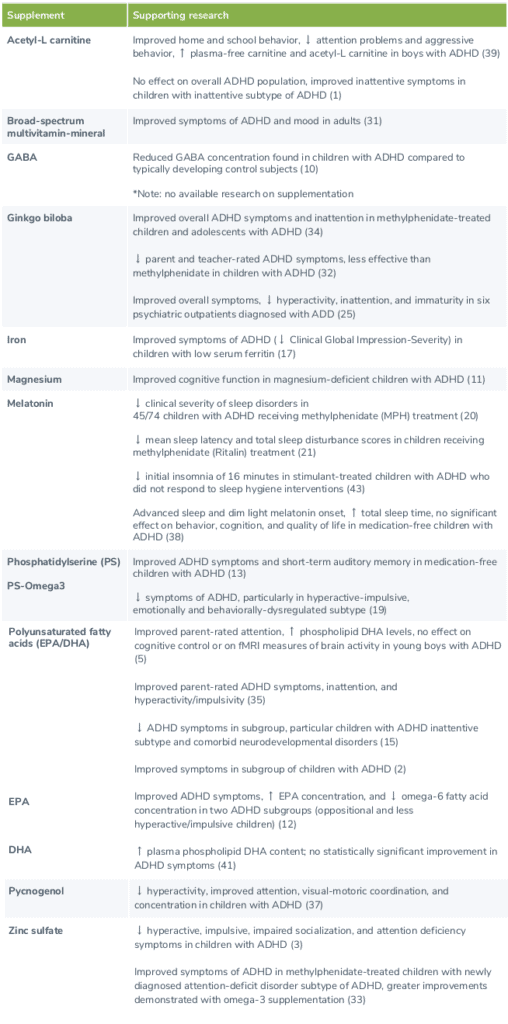
Physical activity and ADHD
While a consensus has not yet been established for frequency, intensity, and duration of exercise, several studies have noted the beneficial effects of exercise programs on symptoms of ADHD and fine motor skills. (24) In a systematic review and meta-analysis of eight randomized controlled trials, both aerobic physical activity and yoga improved ADHD symptoms in children and adolescents, such as attention, hyperactivity, and impulsivity. Additionally, aerobic exercise also improved cognitive function, executive function, anxiety, and social interaction. (8) Similarly, another study examined the effects of physical activity on the cognitive function of 43 children with ADHD between the ages of seven and 12. The children were placed into two experimental groups and a control group; the first experimental group underwent training in ball handling, balance, and manual dexterity, while the second group was trained in sports but did not focus on developing specific skills. After 12 weeks, improvements in working memory, motor performance, and executive function were observed in both experimental groups, indicating that physical activity, regardless of specificity, positively affects children with ADHD. (44) Other studies have found that physical activity improves parent and teacher-observed behavior, as well as muscular capabilities, motor skills, information processing, (40) and reading and arithmetic performance. (30)
Sleep and ADHD
It is estimated that approximately 25-50% of individuals with ADHD experience sleep issues, (21) such as sleep onset difficulties, nighttime awakenings, reduced sleep durations, and bedtime resistance. (42)Did you know? Compared to healthy children, those with ADHD appear to more than twice as likely to develop insomnia, which may exacerbate symptoms of ADHD and mood issues. (21)Insomnia may present itself as a symptom of ADHD, possibly attributed changes in circadian rhythms or melatonin levels. (42) Insomnia may also be an unwanted side-effect of certain medications used to treat ADHD. (9) Children treated with stimulants appear to be twice as likely to develop sleep onset latency or insomnia. (21) Sleep training and maintaining proper sleep hygiene has been shown to benefit children with ADHD. A randomized case-control trial examined the effects of sleep training on the emotional, social, and behavioral functioning of children with ADHD compared to children with ADHD and healthy children who do not receive sleep training. After 12 weeks, those who received training demonstrated improvements in physical and psychosocial well-being, including mood, emotions, and social relationships. (16) A number of sleep habits, which can take months or years to develop, have been suggested to improve sleep hygiene, such as:
- Maintaining a consistent routine and bedtime, gradually reducing energy levels to promote relaxation
- Utilizing relaxation techniques and bedtime “cues”, such as taking a warm bath, drinking a cup of chamomile tea, and engaging in relaxing imagery
- Reducing screen time and other activating stimuli in the bedroom, especially before bed (e.g., tv, video games, loud music)
- Maintaining a comfortable temperature and ventilation in the bedroom
- Engaging in regular physical activity during the day
- If necessary, using sound screens to muffle sounds or eye masks to block light (6)
The bottom line
ADHD is believed to be an epigenetic condition triggered by environmental factors in genetically susceptible individuals. (26) While stimulant medication treatment continues to be the standard, ADHD should be addressed using a multimodal approach. (18) An elimination diet can help to identify trigger foods related to ADHD symptoms. Research has also identified a number of nutrients and botanicals that may be beneficial, including omega-3 fatty acids, phosphatidylserine, acetyl-L carnitine, pycnogenol, ginkgo biloba, melatonin, and certain minerals. Further lifestyle changes, such as engaging in regular physical activity and practicing proper sleep hygiene, may also improve ADHD symptoms and daily functioning.- Arnold, L.E., Amato, A., Bozzolo, H., Hollway, J., Cook, A., Ramadan, Y., … Manos, M. (2007). Acetyl-L-carnitine (ALC) in attention-deficit/hyperactivity disorder: a multi-site, placebo-controlled pilot trial. Journal of Child and Adolescent Psychopharmacology, 17(6), 791-802.
- Bélanger, S. A., Vanasse, M., Spahis, S., Sylvestre, M. P., Lippé, S., L’heureux, F., … Levy, E. (2009). Omega-3 fatty acid treatment of children with attention-deficit hyperactivity disorder: A randomized, double-blind, placebo-controlled study. Paediatrics & Child Health, 14(2), 89–98.
- Bilici, M., Yildirim, F., Kandil, S., Bekaroğlu, M., Yildirmiş, S., Değer, O., … Aksu, H. (2004). Double-blind, placebo-controlled study of zinc sulfate in the treatment of attention deficit hyperactivity disorder. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 28(1), 181-90.
- Bloch, M. H., & Mulqueen, J. (2014). Nutritional supplements for the treatment of ADHD. Child and Adolescent Psychiatric Clinics of North America, 23(4), 883–897.
- Bos, D. J., Oranje, B., Veerhoek, E. S., Van Diepen, R. M., Weusten, J. M., Demmelmair, H., … Durston, S. (2015). Reduced symptoms of inattention after dietary omega-3 fatty acid supplementation in boys with and without attention deficit/hyperactivity disorder. Neuropsychopharmacology, 40(10), 2298–2306.
- Brown, T.E., & McMullen, W.J. (2000). Attention deficit disorders and sleep/arousal disturbance. In T.E. Brown (Ed.), Attention deficit disorders and comorbidities in children, adolescents, and adults (pp. 271-286). Washington, DC: American Psychiatric Press.
- Centers for Disease Control and Prevention. (2018). National prevalence of ADHD and treatment: New statistics for children and adolescents, 2016. Retrieved from https://www.cdc.gov/adhd/data/index.html
- Cerrillo-Urbina, A.J., García-Hermoso, A., Sánchez-López, M., Pardo-Guijarro, M.J., Santos Gómez, J.L., & Martínez-Vizcaíno, V. (2015). The effects of physical exercise in children with attention deficit hyperactivity disorder: a systematic review and meta-analysis of randomized control trials. Child: Care, Health and Development, 41(6), 779-88.
- Cummings, C., & Canadian Paediatric Society, Community Paediatrics Committee. (2012). Melatonin for the management of sleep disorders in children and adolescents. Paediatrics & Child Health, 17(6), 331–336.
- Edden, R. A., Crocetti, D., Zhu, H., Gilbert, D. L., & Mostofsky, S. H. (2012). Reduced GABA concentration in attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 69(7), 750–753.
- El Baza, F., Ahmed AlShahawi, H., Zahra, S., Ahmed, R., & Hakim, A. (2016). Magnesium supplementation in children with attention deficit hyperactivity disorder. Egyptian Journal of Medical Human Genetics, 17(1), 63-70.
- Gustafsson, P.A., Birberg-Thornberg, U., Duchén, K., Landgren, M., Malmberg, K., Pelling, H., … Karlsson, T. (2010). EPA supplementation improves teacher-rated behaviour and oppositional symptoms in children with ADHD. Acta Paediatrica, 99(10), 1540-9.
- Hirayama, S., Terasawa, K., Rabeler, R., Hirayama, T., Inoue, T., Tatsumi, Y., … Jäger, R. (2014). The effect of phosphatidylserine administration on memory and symptoms of attention-deficit hyperactivity disorder: A randomised, double-blind, placebo-controlled clinical trial. Journal of Human Nutrition and Dietetics, 27(Suppl 2), 284-91.
- Institute for Quality and Efficiency in Health Care (IQWiG). (2015). InformedHealth.org . Cologne, Germany: Author.
- Johnson, M., Ostlund, S., Fransson, G., Kadesjö, B., & Gillberg, C. (2009). Omega-3/omega-6 fatty acids for attention deficit hyperactivity disorder: A randomized placebo-controlled trial in children and adolescents. Journal of Attention Disorders, 12(5), 394-401.
- Keshavarzi, Z., Bajoghli, H., Mohamadi, M.R., Salmanian, M., Kirov, R., Gerber, M., … Brand, S. (2014). In a randomized case–control trial with 10-years olds suffering from attention deficit/hyperactivity disorder (ADHD) sleep and psychological functioning improved during a 12-week sleep-training program. The World Journal of Biological Psychiatry, 15(8), 609-619.
- Konofal, E., Lecendreux, M., Deron, J., Marchand, M., Cortese, S., Zaïm, M., … Arnulf, I. (2008). Effects of iron supplementation on attention deficit hyperactivity disorder in children. Pediatric Neurology, 38(1), 20-6.
- Madzhidova, S., & Sedrakyan, L. (2019). The use of dietary interventions in pediatric patients. Pharmacy (Basel, Switzerland), 7(1), 10.
- Manor, I., Magen, A., Keidar, D., Rosen, S., Tasker, H., Cohen, T., … Weizman, A. (2012). The effect of phosphatidylserine containing Omega3 fatty-acids on attention-deficit hyperactivity disorder symptoms in children: A double-blind placebo-controlled trial, followed by an open-label extension. European Psychiatry, 27(5), 335-42.
- Masi, G., Fantozzi, P., Villafranca, A., Tacchi, A., Ricci, F., Ruglioni, L., … Cortese, S. (2019). Effects of melatonin in children with attention-deficit/hyperactivity disorder with sleep disorders after methylphenidate treatment. Neuropsychiatric Disease and Treatment, 15, 663–667.
- Mohammadi, M. R., Mostafavi, S. A., Keshavarz, S. A., Eshraghian, M. R., Hosseinzadeh, P., Hosseinzadeh-Attar, M. J., … Akhondzadeh, S. (2012). Melatonin effects in methylphenidate treated children with attention deficit hyperactivity disorder: a randomized double blind clinical trial. Iranian Journal of Psychiatry, 7(2), 87–92.
- National Institute of Mental Health. (2016). Attention-deficit/hyperactivity disorder. Retrieved from https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd/index.shtml
- National Institute of Mental Health. (2017). Attention-deficit/hyperactivity disorder (ADHD). Retrieved from https://www.nimh.nih.gov/health/statistics/attention-deficit-hyperactivity-disorder-adhd.shtml
- Neudecker, C., Mewes, N, Reimers, A.K., & Woll, A. (2015). Exercise interventions in children and adolescents with ADHD: A systematic review. Journal of Attention Disorders, 23(4).
- Niederhofer, H. (2010). Ginkgo biloba treating patients with attention‐deficit disorder. Phytotherapy Research, 24(1), 26-27.
- Nigg, J. T., & Holton, K. (2014). Restriction and elimination diets in ADHD treatment. Child and Adolescent Psychiatric Clinics of North America, 23(4), 937–953.
- Nigg, J. T., Lewis, K., Edinger, T., & Falk, M. (2012). Meta-analysis of attention-deficit/hyperactivity disorder or attention-deficit/hyperactivity disorder symptoms, restriction diet, and synthetic food color additives. Journal of the American Academy of Child and Adolescent Psychiatry, 51(1), 86–97.e8.
- Pelsser, L.M., Frankena, K., Toorman, J., Savelkoul, H.F., Dubois, A.E., Pereira, R.R., … Buitelaar, J.K. (2011). Effects of a restricted elimination diet on the behaviour of children with attention-deficit hyperactivity disorder (INCA study): A randomised controlled trial. Lancet, 377(9764), 494-503.
- Pelsser, L.M. J., Frankena, K., Toorman, J., Savelkoul, H.F. J., Rodrigues Pereira, R., & Buitelaar, J.K. (2009). A randomised controlled trial into the effects of food on ADHD. European Child & Adolescent Psychiatry, 18(1), 12–19.
- Pontifex, M. B., Saliba, B. J., Raine, L. B., Picchietti, D. L., & Hillman, C. H. (2013). Exercise improves behavioral, neurocognitive, and scholastic performance in children with attention-deficit/hyperactivity disorder. The Journal of Pediatrics, 162(3), 543–551.
- Rucklidge, J.J., Frampton, C.M., Gorman, B., & Boggis, A. (2014). Vitamin-mineral treatment of attention-deficit hyperactivity disorder in adults: double-blind randomised placebo-controlled trial. British Journal of Psychiatry, 204, 306-15.
- Salehi, B., Imani, R., Mohammadi, M.R., Fallah, J., Mohammadi, M., Ghanizadeh, A., … Akhondzadeh, S. (2010). Ginkgo biloba for Attention-Deficit/Hyperactivity Disorder in children and adolescents: A double blind, randomized controlled trial. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 34(1), 76-80.
- Salehi, B., Mohammadbeigi, A., Sheykholeslam, H., Moshiri, E., & Dorreh, F. (2016). Omega-3 and zinc supplementation as complementary therapies in children with attention-deficit/hyperactivity disorder. Journal of Research in Pharmacy Practice, 5(1), 22–26.
- Shakibaei, F., Radmanesh, M., Salari, E., & Mahaki, B. (2015). Ginkgo biloba in the treatment of attention-deficit/hyperactivity disorder in children and adolescents. A randomized, placebo-controlled, trial. Complementary Therapies in Clinical Practice, 21(2), 61-7.
- Sinn, N., & Bryan, J. (2007). Effect of supplementation with polyunsaturated fatty acids and micronutrients on learning and behavior problems associated with child ADHD. Journal of Developmental and Behavioral Pediatrics, 28(2), 82-91.
- Stevens, L.J., Kuczek, T. Burgess, J.R., Hurt, E., & Arnold, L.E. (2010). Dietary sensitivities and ADHD symptoms: Thirty-five years of research. Clinical Pediatrics, 50(4), 279-293.
- Trebatická, J., Kopasová, S., Hradecná, Z., Cinovský, K., Skodácek, I., Suba, J., … Duracková, Z. (2006). Treatment of ADHD with French maritime pine bark extract, Pycnogenol. European Child & Adolescent Psychiatry, 15(6), 329-35.
- Van der Heijden, K., Smits, M.G., Van Someren, E.J.W., Ridderinkhof, R., & Boudewijn Gunning, W. (2007). Effect of melatonin on sleep, behavior, and cognition in ADHD and chronic sleep-onset insomnia. Journal of the American Academy of Child & Adolescent Psychiatry, 46(2), 233-241.
- Van Oudheusden, L.J., & Scholte, H.R. (2002). Efficacy of carnitine in the treatment of children with attention-deficit hyperactivity disorder. Prostaglandins Leukotrienes Essential Fatty Acids, 67(1), 33-8.
- Verret, C., Guay, M., Berthiaume, C., Gardiner, P., Béliveau, L. (2012). A physical activity program improves behavior and cognitive functions in children with ADHD: An exploratory study. Journal of Attention Disorders, 16(1), 71-80.
- Voigt, R.G., Llorente, A.M., Jensen, C.L., Fraley, J.K., Berretta, M.C., & Heird, W.C. (2001). A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. The Journal of Pediatrics, 139(2), 189-96.
- Weissenberger, S., Ptacek, R., Klicperova-Baker, M., Erman, A., Schonova, K., Raboch, J., & Goetz, M. (2017). ADHD, lifestyles and comorbidities: A call for an holistic perspective – from medical to societal intervening factors. Frontiers in Psychology, 8, 454.
- Weiss, M.D., Wasdell, M.B., Bomben, M.M., Rea, K.J., & Freeman, R.D. (2006). Sleep hygiene and melatonin treatment for children and adolescents with ADHD and initial insomnia. Journal of the American Academy of Child and Adolescent Psychiatry, 45(5), 512-9.
- Ziereis, S., & Jansen, P. (2015). Effects of physical activity on executive function and motor performance in children with ADHD. Research in Developmental Disabilities, 38, 181-191.





