What are adrenal glands?
The adrenal glands are small, triangular-shaped organs found on top of the kidneys. They’re responsible for producing several important hormones, including cortisol, aldosterone, dehydroepiandrosterone (DHEA), androgenic steroids, norepinephrine, and epinephrine. These hormones help regulate your immune system, metabolism, blood pressure, response to stress, and other essential functions. (26)(32) If your adrenal glands are not functioning properly, they may over or underproduce these hormones, which can lead to several health issues. (48)What is adrenal fatigue?
Adrenal fatigue is a term most commonly used by integrative healthcare providers and functional doctors to describe a collection of symptoms believed to be induced by chronic stress. (49) It’s important to note that adrenal fatigue is not an accepted medical diagnosis. Instead, you may also hear adrenal fatigue referred to as hypothalamic pituitary adrenal (HPA) axis dysfunction. The two terms are often used interchangeably. (4)(46)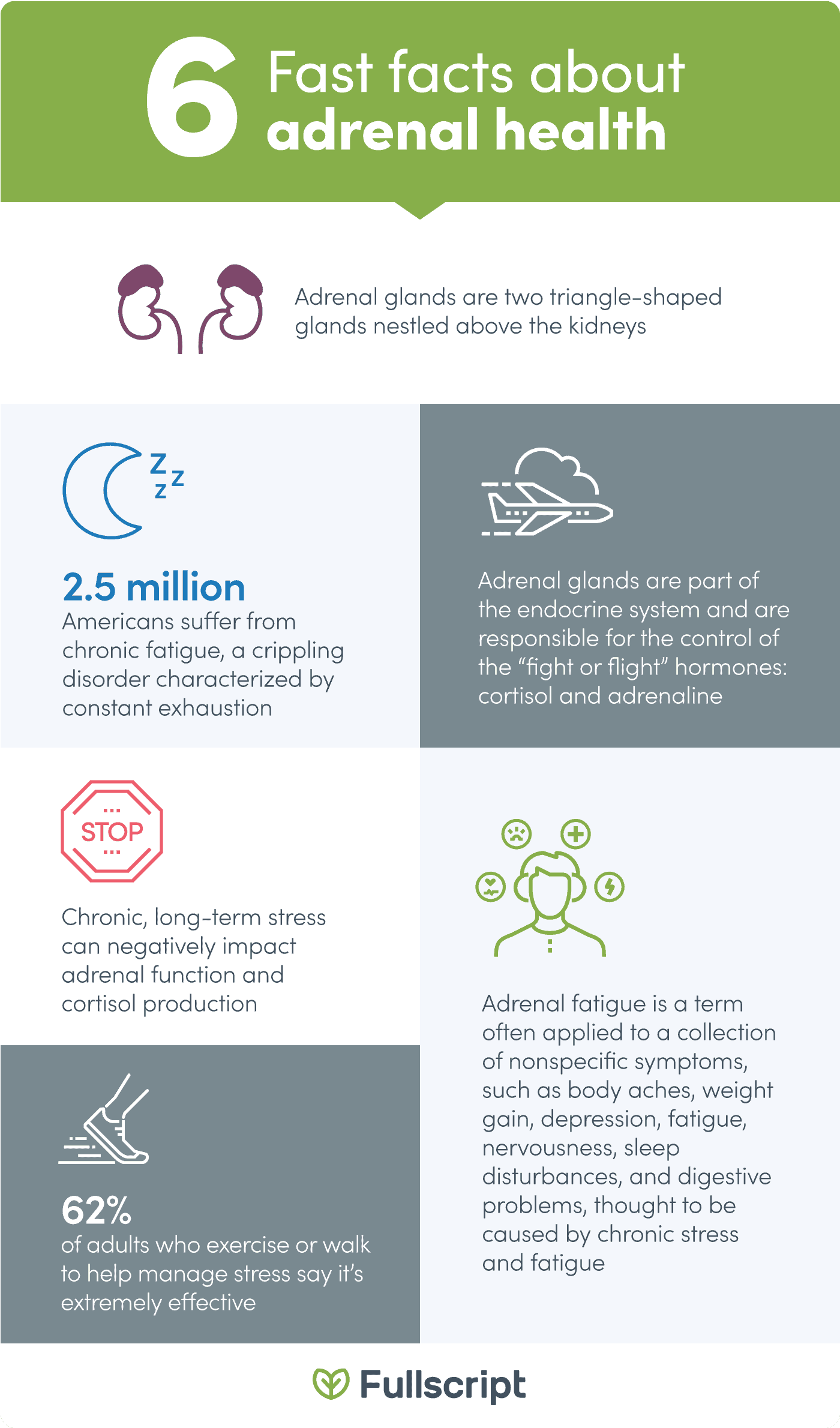
Get the facts about adrenal health. The references for this infographic are listed in the section titled “Infographic references”, below.
Identifying adrenal fatigue
Symptoms often associated with adrenal fatigue include:- Cognitive deficits
- Decreased libido
- Depression
- Fatigue
- Hormone imbalances
- Hypoglycemia
- Hypertension
- Insulin resistance
- Irritability
- Poor stress coping skills
- Sleep issues
- Weight gain (2)(13)(14)(16)(49)

Feeling constantly tired is just one symptom of adrenal fatigue.
What is adrenal insufficiency disorder?
Adrenal insufficiency, also known as Addison’s disease, is a recognized autoimmune disorder characterized by insufficient hormone production that occurs when adrenal glands don’t make enough of certain hormones. (29) Some integrative healthcare practitioners consider adrenal fatigue to be a mild form of adrenal insufficiency, however, the symptoms differ slightly. Adrenal insufficiency symptoms include:- Abdominal pain
- Chronic fatigue
- Darkening of the skin
- Diarrhea
- Hypoglycemia (low blood glucose)
- Irregular menstrual cycles
- Joint pain
- Low blood pressure
- Low libido
- Muscle weakness
- Nausea and vomiting
- Poor appetite
- Weight loss (30)
Top natural strategies for supporting adrenal health
Incorporate these five simple strategies into your daily routine to help support your adrenal function.
Dr. Holly Lucille ND, RN, discusses the ins and outs of Adrenal fatigue and HPA axis dysfunction.Eat nutritious foods
Although there is no specific diet for treating or reducing the risk of adrenal fatigue, eating a healthy, well-balanced diet may help support adrenal health and promote general well-being. Research suggests that the Mediterranean diet, which focuses on the intake of vegetables, fruits, legumes, nuts, seeds, grains, fish, dairy, and moderate amounts of meat and poultry, may be the best diet for overall health and may reduce stress-induced inflammation. (5) Furthermore, individuals should limit their intake of coffee and other caffeinated foods and beverages, as high doses of caffeine can increase cortisol secretion and activate the HPA axis. (24)(36)Aim for daily exercise
Research has found that regular exercise can combat stress and help you establish emotional resilience in response to acute stress. (7) The National Institutes of Health recommends that adults engage in at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity aerobic exercise per week. Strength training sessions twice per week is also encouraged. (47)Get enough quality sleep
Did you know that poor quality sleep can negatively impact how your body responds to stress? (28) Research has demonstrated a possible link between inadequate sleep and increased cortisol levels. (1) According to the National Sleep Foundation, young adults should aim to get between seven to nine hours of sleep and older adults should get between seven to eight hours of sleep per night. (18) To support optimal sleep, maintain a regular sleep schedule, minimize external sources of light and sound around bedtime, and engage in regular physical activity. (11)(19)Practice meditation
Meditation is a practice that can help reduce stress, improve overall well-being, and encourage a heightened state of awareness, focus, and relaxation. (43) One study investigated the effects of meditation on stress and found that meditation significantly reduced the change in cortisol levels in the first hour of waking, known as the cortisol awakening response (CAR), compared to the control group. (23)Consider taking adrenal support supplements
When advised by a healthcare practitioner, taking certain supplements, such as ashwagandha, rhodiola, Panax ginseng, and vitamin C, may help support the health of your adrenal glands. Individuals with adrenal gland issues may experience high levels of certain hormones, while others may experience low levels. (31) Depending on your condition, your practitioner may recommend a protocol of specific supplements. Learn more about supplements for adrenal health on the Fullscript blog.The bottom line
The adrenal glands are small glands located on the kidneys that produce and control the secretion of several hormones. Chronic stress can negatively impact adrenal gland function, which can contribute to the development of certain health conditions. Managing your stress through lifestyle modifications, as well as supplementation when directed by your integrative healthcare practitioner, may help support overall adrenal health.- Balbo, M., Leproult, R., & Van Cauter, E. (2010). Impact of sleep and its disturbances on hypothalamo-pituitary-adrenal axis activity. International Journal of Endocrinology, 2010, 1–16.
- Basson, R., O’Loughlin, J. I., Weinberg, J., Young, A. H., Bodnar, T., & Brotto, L. A. (2019). Dehydroepiandrosterone and cortisol as markers of HPA axis dysregulation in women with low sexual desire. Psychoneuroendocrinology, 104, 259–268.
- Brody, S., Preut, R., Schommer, K., & Schürmeyer, T. H. (2001). A randomized controlled trial of high dose ascorbic acid for reduction of blood pressure, cortisol, and subjective responses to psychological stress. Psychopharmacology, 159(3), 319–324.
- Cadegiani, F. A., & Kater, C. E. (2016). Adrenal fatigue does not exist: a systematic review. BMC Endocrine Disorders, 16(1), 48.
- Carvalho, K., Ronca, D., Michels, N., Huybrechts, I., Cuenca-Garcia, M., Marcos, A., … Carvalho, L. (2018). Does the mediterranean diet protect against stress-induced inflammatory activation in European adolescents? The HELENA study. Nutrients, 10(11), 1770.
- Chandrasekhar, K., Kapoor, J., & Anishetty, S. (2012). A prospective, randomized double-blind, placebo-controlled study of safety and efficacy of a high-concentration full-spectrum extract of Ashwagandha root in reducing stress and anxiety in adults. Indian Journal of Psychological Medicine, 34(3), 255–262.
- Childs, E., & de Wit, H. (2014). Regular exercise is associated with emotional resilience to acute stress in healthy adults. Frontiers in Physiology, 5, 161.
- Cohen, M. (2014). Tulsi – Ocimum sanctum: A herb for all reasons. Journal of Ayurveda and Integrative Medicine, 5(4), 251–259.
- DiNicolantonio, J. J., O’Keefe, J. H., & Wilson, W. (2018). Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open Heart, 5(1), e000668.
- Flanagan, S. D., DuPont, W. H., Caldwell, L. K., Hardesty, V. H., Barnhart, E. C., Beeler, M. K., … Kraemer, W. J. (2018). The effects of a Korean ginseng, GINST15, on hypo-pituitary-adrenal and oxidative activity induced by intense work stress. Journal of Medicinal Food, 21(1), 104–112.
- Flausino, N. H., Da Silva Prado, J. M., Queiroz, S. S., Tufik, S., & Mello, M. T. (2011). Physical exercise performed before bedtime improves the sleep pattern of healthy young good sleepers. Psychophysiology, 49(2), 186–192.
- Gröber, U., Schmidt, J., & Kisters, K. (2015). Magnesium in prevention and therapy. Nutrients, 7(9), 8199–8226.
- Hannibal, K. E., & Bishop, M. D. (2014). Chronic stress, cortisol dysfunction, and pain: A psychoneuroendocrine rationale for stress management in pain rehabilitation. Physical Therapy, 94(12), 1816–1825.
- Harbuz, M. (2002). Neuroendocrine Function and Chronic Inflammatory Stress. Experimental Physiology, 87(5), 519–525.
- Hellhammer, J., Vogt, D., Franz, N., Freitas, U., & Rutenberg, D. (2014). A soy-based phosphatidylserine/ phosphatidic acid complex (PAS) normalizes the stress reactivity of hypothalamus-pituitary-adrenal-axis in chronically stressed male subjects: a randomized, placebo-controlled study. Lipids in Health and Disease, 13(1), 121.
- Hewagalamulage, S. D., Lee, T. K., Clarke, I. J., & Henry, B. A. (2016). Stress, cortisol, and obesity: a role for cortisol responsiveness in identifying individuals prone to obesity. Domestic Animal Endocrinology, 56, S112–S120.
- Hill, E. E., Zack, E., Battaglini, C., Viru, M., Viru, A., & Hackney, A. C. (2008). Exercise and circulating cortisol levels: The intensity threshold effect. Journal of Endocrinological Investigation, 31(7), 587–591.
- Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C., Bruni, O., DonCarlos, L., … Adams Hillard, P. J. (2015). National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health, 1(1), 40–43.
- Irish, L. A., Kline, C. E., Gunn, H. E., Buysse, D. J., & Hall, M. H. (2015). The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Medicine Reviews, 22, 23–36.
- Jamshidi, N., & Cohen, M. M. (2017). The clinical efficacy and safety of tulsi in humans: A systematic review of the literature. Evidence-Based Complementary and Alternative Medicine, 2017, 1–13.
- Kim, H.-G., Cho, J.-H., Yoo, S.-R., Lee, J.-S., Han, J.-M., Lee, N.-H., … Son, C.-G. (2013). Antifatigue effects of Panax ginseng C.A. Meyer: A randomised, double-blind, placebo-controlled trial. PLoS ONE, 8(4), e61271.
- Kim, J.-H. (2018). Pharmacological and medical applications of Panax ginseng and ginsenosides: a review for use in cardiovascular diseases. Journal of Ginseng Research, 42(3), 264–269.
- Klimes-Dougan, B., Chong, L. S., Samikoglu, A., Thai, M., Amatya, P., Cullen, K. R., & Lim, K. O. (2019). Transcendental meditation and hypothalamic-pituitary-adrenal axis functioning: a pilot, randomized controlled trial with young adults. Stress, 23(1), 105–115.
- Lovallo, W. R., Whitsett, T. L., al’Absi, M., Sung, B. H., Vincent, A. S., & Wilson, M. F. (2005). Caffeine stimulation of cortisol secretion across the waking hours in relation to caffeine intake levels. Psychosomatic Medicine, 67(5), 734–739.
- Mariotti, A. (2015). The effects of chronic stress on health: new insights into the molecular mechanisms of brain–body communication. Future Science OA, 1(3), 23.
- Megha, R., Wehrle, C. J., Kashyap, S., & Leslie, S. W. (2020). Anatomy, abdomen and pelvis, adrenal glands (suprarenal glands). StatPearls.
- Michels, A. W., & Eisenbarth, G. S. (2010). Immunologic endocrine disorders. Journal of Allergy and Clinical Immunology, 125(2), S226–S237.
- Mohammadi, H., Rezaei, M., Amiri, S. M., Rahimi, Z., Mansouri, K., & Khazaie, H. (2018). Sleep architecture and hypothalamic-pituitary-adrenal activity in paradoxical and psychophysiological insomnia. Basic and Clinical Neuroscience Journal, 9(6), 397–407.
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020a, July 15). Adrenal insufficiency & Addison’s disease. https://www.niddk.nih.gov/health-information/endocrine-diseases/adrenal-insufficiency-addisons-disease
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020b, July 15). Symptoms and causes of adrenal insufficiency & Addison’s disease. https://www.niddk.nih.gov/health-information/endocrine-diseases/adrenal-insufficiency-addisons-disease/symptoms-causes
- National Institutes of Health. (2017, January 31). How do health care providers diagnose adrenal gland disorders? https://www.nichd.nih.gov/health/topics/adrenalgland/conditioninfo/diagnosed
- Nussey, S. (2001). The adrenal gland. In S. Whitehead (Ed.), Endocrinology: An Integrated Approach (p. 1). https://www.ncbi.nlm.nih.gov/books/NBK26/
- Olsson, E., von Schéele, B., & Panossian, A. (2008). A randomised, double-blind, placebo-controlled, parallel-group study of the standardised extract SHR-5 of the roots of rhodiola rosea in the treatment of subjects with stress-related fatigue. Planta Medica, 75(02), 105–112.
- Padayatty, S. J., Doppman, J. L., Chang, R., Wang, Y., Gill, J., Papanicolaou, D. A., & Levine, M. (2007). Human adrenal glands secrete vitamin C in response to adrenocorticotrophic hormone. The American Journal of Clinical Nutrition, 86(1), 145–149.
- Patak, P., Willenberg, H. S., & Bornstein, S. R. (2004). Vitamin C Is an important cofactor for both adrenal cortex and adrenal medulla. Endocrine Research, 30(4), 871–875.
- Patz, M. D., Day, H. E. W., Burow, A., & Campeau, S. (2006). Modulation of the hypothalamo–pituitary–adrenocortical axis by caffeine. Psychoneuroendocrinology, 31(4), 493–500.
- Poleszak, E., Szewczyk, B., Kędzierska, E., Wlaź, P., Pilc, A., & Nowak, G. (2004). Antidepressant- and anxiolytic-like activity of magnesium in mice. Pharmacology Biochemistry and Behavior, 78(1), 7–12.
- Reddy, P., & Jialal, I. (Eds.). (2018). Biochemistry, Vitamin, Fat Soluble. https://www.ncbi.nlm.nih.gov/books/NBK534869/
- Rolf, L., Damoiseaux, J., Huitinga, I., Kimenai, D., van den Ouweland, J., Hupperts, R., & Smolders, J. (2018). Stress-axis regulation by vitamin D3 in multiple sclerosis. Frontiers in Neurology, 9, 263.
- Sampath, S., Mahapatra, S. C., Padhi, M. M., Sharma, R., & Talwar, A. (2015). Holy basil (Ocimum sanctum Linn.) leaf extract enhances specific cognitive parameters in healthy adult volunteers: A placebo controlled study. Indian J Physiol Pharmacol ., 59(1), 69–77.
- Sartori, S. B., Whittle, N., Hetzenauer, A., & Singewald, N. (2012). Magnesium deficiency induces anxiety and HPA axis dysregulation: Modulation by therapeutic drug treatment. Neuropharmacology, 62(1), 304–312.
- Schwalfenberg, G. K., & Genuis, S. J. (2017). The importance of magnesium in clinical healthcare. Scientifica, 2017, 1–14.
- Sharma, H. (2015). Meditation: Process and effects. AYU (An International Quarterly Journal of Research in Ayurveda), 36(3), 233–237.
- Singh, N., Bhalla, M., De Jager, P., & Gilca, M. (2011). An overview on ashwagandha: A rasayana (Rejuvenator) of ayurveda. African Journal of Traditional, Complementary and Alternative Medicines, 8(5S), 208–213.
- Smith, S. M., Vale, W. W., & Mondal, A. C. (2006). The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues Clin Neurosci, 8(4), 383–395.
- Tomas, C., Newton, J., & Watson, S. (2013). A review of hypothalamic-pituitary-adrenal axis function in chronic fatigue syndrome. ISRN Neuroscience, 2013, 1–8.
- U.S. National Library of Medicine. (2017, August 30). How much exercise do I need? https://medlineplus.gov/howmuchexercisedoineed.html
- U.S. National Library of Medicine. (2018, May 8). Adrenal gland disorders. Retrieved from https://medlineplus.gov/adrenalglanddisorders.html
- Wilson, J. L. (2014). Clinical perspective on stress, cortisol and adrenal fatigue. Advances in Integrative Medicine, 1(2), 93–96.
- Yeo, K. J., Babic, N., Hannoush, Z. C., & Weiss, R. E. (2017). Endotext. Endocrine Testing Protocols: Hypothalamic Pituitary Adrenal Axis.





