What is a fertility awareness-based method?
A fertility awareness-based method (FABM) refers to a non-pharmaceutical family planning tactic used to prevent or improve the chances of conception through ovulation detection. (11)(12) Ovulation is the process in which one of your ovaries releases a mature egg, which typically occurs between days 12 and 16 in an average cycle. (11) Once an egg is released, it must be fertilized within 24 hours after ovulation in order to achieve pregnancy. (15) With male sperm staying alive in the female body for up to five days, the fertile window is approximately six days for most premenopausal women. (5)(24)(26) FABM involves tracking your cycle through various methods, such as basal body temperature (BBT) and cervical secretions, to detect future ovulation. These methods can help you prevent conception by determining your most fertile days during which it’s best to either abstain from intercourse or use barrier contraception (e.g., condoms). (15) Using this method as a form of birth control requires research, self-awareness, and diligence in order to be successful. (6)Trying to conceive? FABMs can also be used to achieve pregnancy. By identifying your fertile window, you can determine the best time to have sex to optimize your chances of conceiving.

This greater awareness of your own body through fertility awareness methods can lead to greater intimacy with your partner. (6)(25)
Types of fertility awareness methods
From the basal body temperature (BBT) fertility method to the cervical secretion method, there are many approaches that allow you to gain a deeper understanding of your body in order to prevent unwanted pregnancy.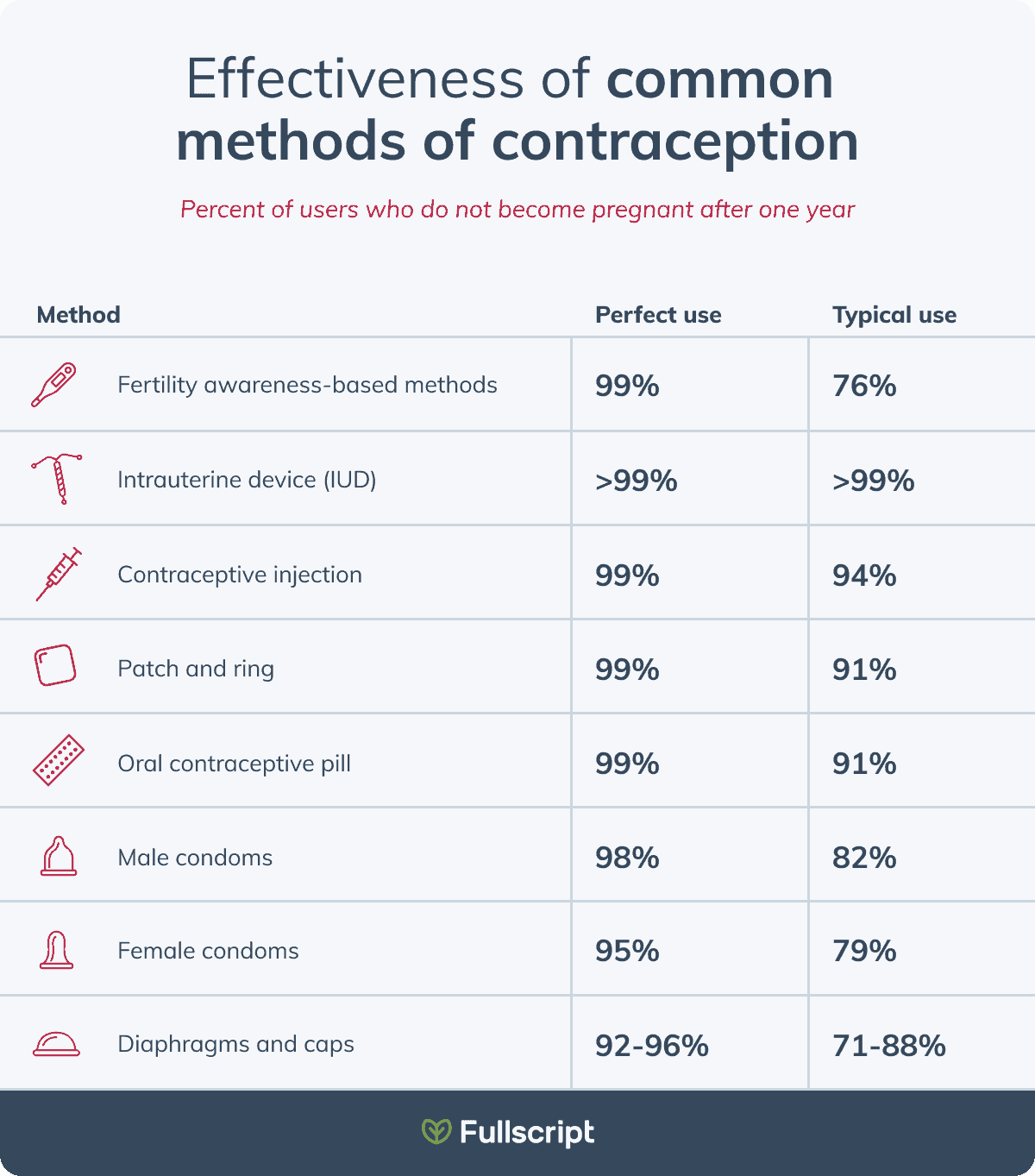
Learn how fertility awareness-based methods compare to other common contraceptive methods. (14)
1. Basal body temperature
The basal body temperature (BBT) fertility awareness method uses body temperature measurements to track ovulation and predict your fertile window. BBT refers to your internal resting body temperature, and this fertility awareness method involves taking your temperature first thing in the morning before getting out of bed, providing the most accurate reading. Since fluctuations are slight, it is important to use a basal body thermometer that records 2 decimal places for an accurate temperature reading. (22) Your basal body temperature is lowest during the first half of your cycle, increasing during ovulation. (22) With this method, it is recommended that you track at least six to 12 cycles before you can trust the results. (12) When misused, 24 out of 100 women become pregnant each year. (18) Download a BBT tracker handout in Fahrenheit and Celsius.2. Standard days method
The standard days method involves tracking your cycle using a calendar and refraining from intercourse or using barrier protection from days eight through 19 of the menstrual cycle. (1) A pregnancy rate of 4.75% with correct use and 11.96% with typical use suggests that this method can be successful in natural pregnancy prevention. (1) This method works best for women with regular and predictable cycles. (8)3. Cervical secretion method
The cervical secretion method is another way of determining your fertile window, achieved through documenting changes in the physical characteristics of cervical fluid. (10)(20) Cervical fluid is essential to transporting sperm for successful fertilization. Its properties and consistency change throughout the menstrual cycle corresponding with ovulation. (10) Mucus consistency can be described as creamy and white, to a slippery, egg white consistency depending on what stage you are in your cycle. The days where mucus can be described as having an egg white consistency often means ovulation is about to occur. (4) Awareness of fertile cervical mucus during ovulation, in combination with other markers such as BBT, can help predict fertility periods. (4)4. The symptothermal method
The symptothermal method of fertility awareness combines elements from the BBT, standard days, and cervical mucus methods. (15) When used consistently and accurately, tracking temperature, secretions, and abstaining from unprotected intercourse during the fertile window, the symptothermal method can be an effective method of natural family planning with a pregnancy rate of 0.6 per 100 women. (7)5. Luteinizing hormone tests
Testing urinary luteinizing hormone (LH) levels is another effective way to detect ovulation when used in combination with other methods of fertility awareness. (9) At-home test strips can be used to identify spikes in LH levels that occur during ovulation. Raised levels of urinary LH have been linked to a 100% correlation with the process of ovulation. (9)
The basal body temperature fertility awareness method involves taking your temperature first thing in the morning before getting out of bed for the most accurate reading. (22)
Benefits of fertility awareness-based methods
There are many benefits to using fertility awareness-based methods for birth control. While pharmaceutical contraceptives can have a negative impact on physical, emotional, and sexual wellbeing, FABMs do not involve any medication or synthetic hormones, and therefore have no reported associated side effects. (15)(19) This low-cost contraceptive method also ensures no consequences when planning for pregnancy in the future since this method doesn’t interrupt natural hormone fluctuations with synthetic hormones. (3) FABMs also empower individuals to gain awareness and knowledge about their own health and fertility, which may lead to more intimacy and open communication with your partner. (6)(25) If used consistently, FABMs can be an effective form of contraception with less than a 5% unwanted pregnancy rate, comparable to other commonly used birth control methods such as condoms and the birth control pill. (13)
A luteinizing hormone test is another effective way to detect ovulation. (9)
Apps to help you track
Using a mobile app to help track your fertility can increase adherence and lead to more consistent, accurate tracking. (2) Examples of highly-rated apps currently available on either the App Store or Google Play Store include:- Apple Health
- Natural Cycles
- Clue
- Flo
Did you know? Natural Cycles is the only U.S. Food and Drug Administration-approved birth control app. (16)
Disadvantages of FABMs
Along with the benefits of FABMs, there are also some disadvantages to consider when determining if this form of contraception is right from you, including:- Decreases intercourse spontaneity during the fertile window
- Does not protect against sexually transmitted diseases (17)
- Increases risk for unintended pregnancy compared to other methods (e.g., birth control pill, IUD, patches, condoms)
- Not recommended for premenopausal women who have irregular periods (15)
- Requires consistent tracking of your symptoms for at least six cycles to ensure reliability (12)
The bottom line
Fertility awareness based methods offer side effect-free contraception through ovulation detection. (11)(12) From BBT, standard days, cervical secretions, and symptothermal methods to luteinizing hormone testing, fertility awareness can be an empowering form of birth control that can improve your health, self-awareness, and relationship with your partner. However, it’s important to keep in mind that these approaches require diligence and consistency in order to be effective. When considering contraception, speak to your integrative healthcare practitioner about the numerous options available to you.JTVCYmxvZy1jdGElNUQlMEE=[/vc_raw_html]- Arévalo, M., Jennings, V., & Sinai, I. (2002). Efficacy of a new method of family planning: The Standard Days Method. Contraception, 65(5), 333–338.
- Berglund Scherwitzl, E., Lundberg, O., Kopp Kallner, H., Gemzell Danielsson, K., Trussell, J., & Scherwitzl, R. (2017). Perfect-use and typical-use Pearl Index of a contraceptive mobile app. Contraception, 96(6), 420–425.
- Berglund Scherwitzl, E., Lundberg, O., Kopp Kallner, H., Rowland, S. P., Holte, J., Trussell, J., Gemzell Danielsson, K., & Scherwitzl, R. (2019). Short- and long-term effect of contraceptive methods on fecundity. The European Journal of Contraception & Reproductive Health Care: The Official Journal of the European Society of Contraception, 24(4), 260–265.
- Bigelow, J. L., Dunson, D. B., Stanford, J. B., Ecochard, R., Gnoth, C., & Colombo, B. (2004). Mucus observations in the fertile window: A better predictor of conception than timing of intercourse. Human Reproduction , 19(4), 889–892.
- Dunson, D. B., Baird, D. D., Wilcox, A. J., & Weinberg, C. R. (1999). Day-specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation. Human Reproduction , 14(7), 1835–1839.
- Flynn, A. M. (1984). Natural methods of family planning. Clinics in Obstetrics and Gynaecology, 11(3), 661–678.
- Frank-Herrmann, P., Heil, J., Gnoth, C., Toledo, E., Baur, S., Pyper, C., Jenetzky, E., Strowitzki, T., & Freundl, G. (2007). The effectiveness of a fertility awareness based method to avoid pregnancy in relation to a couple’s sexual behaviour during the fertile time: A prospective longitudinal study. Human Reproduction , 22(5), 1310–1319.
- Gribble, J. N., Lundgren, R. I., Velasquez, C., & Anastasi, E. E. (2008). Being strategic about contraceptive introduction: The experience of the Standard Days Method. Contraception, 77(3), 147–154.
- Guida, M., Tommaselli, G. A., Palomba, S., Pellicano, M., Moccia, G., Di Carlo, C., & Nappi, C. (1999). Efficacy of methods for determining ovulation in a natural family planning program. Fertility and Sterility, 72(5), 900–904.
- Katz, D. F. (1991). Human cervical mucus: Research update. American Journal of Obstetrics and Gynecology, 165(6 Pt 2), 1984–1986.
- Klaus, H. (1982). Natural family planning: A review. Obstetrical & Gynecological Survey, 37(2), 128–150.
- Kleinschmidt, T. K., Bull, J. R., Lavorini, V., Rowland, S. P., Pearson, J. T., Scherwitzl, E. B., Scherwitzl, R., & Danielsson, K. G. (2019). Advantages of determining the fertile window with the individualised Natural Cycles algorithm over calendar-based methods. The European Journal of Contraception & Reproductive Health Care: The Official Journal of the European Society of Contraception, 24(6), 457–463.
- Manhart, M. D., Duane, M., Lind, A., Sinai, I., & Golden-Tevald, J. (2013). Fertility awareness-based methods of family planning: A review of effectiveness for avoiding pregnancy using SORT. Osteopathic Family Physician, 5(1), 2–8.
- NHS England. (2020). How effective is contraception at preventing pregnancy? https://www.nhs.uk/conditions/contraception/how-effective-contraception/
- Pallone, S. R., & Bergus, G. R. (2009). Fertility awareness-based methods: Another option for family planning. Journal of the American Board of Family Medicine: JABFM, 22(2), 147–157.
- Pearson, J. T., Chelstowska, M., Rowland, S. P., Benhar, E., Kopp-Kallner, H., Berglund Scherwitzl, E., Acuna, J., … & Scherwitzl, R. (2021). Contraceptive effectiveness of an FDA-cleared birth control app: Results from the natural cycles U.S. cohort. Journal of Women’s Health , 30(6), 782–788.
- Pedro, J., Brandão, T., Schmidt, L., Costa, M. E., & Martins, M. V. (2018). What do people know about fertility? A systematic review on fertility awareness and its associated factors. Upsala Journal of Medical Sciences, 123(2), 71–81.
- Planned Parenthood. (n.d.). Fertility awareness. https://www.plannedparenthood.org/learn/birth-control/fertility-awareness
- Sanders, S. A., Graham, C. A., Bass, J. L., & Bancroft, J. (2001). A prospective study of the effects of oral contraceptives on sexuality and well-being and their relationship to discontinuation. Contraception, 64(1), 51–58.
- Scarpa, B., Dunson, D. B., & Colombo, B. (2006). Cervical mucus secretions on the day of intercourse: An accurate marker of highly fertile days. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 125(1), 72–78.
- Stanford, J. B., Thurman, P. B., & Lemaire, J. C. (1999). Physicians’ knowledge and practices regarding natural family planning. Obstetrics & Gynecology, 94(5, Part 1), 672–678.
- Steward, K., & Raja, A. (2021). Physiology, ovulation and basal body temperature. In StatPearls. StatPearls Publishing.
- United Nations. Department of International Economic and Social Affairs. (1989). Levels and trends of contraceptive use as assessed in 1988: Vol. no. 110. UN.
- Wilcox, A. J., Weinberg, C. R., & Baird, D. D. (1995). Timing of sexual intercourse in relation to ovulation. Effects on the probability of conception, survival of the pregnancy, and sex of the baby. The New England Journal of Medicine, 333(23), 1517–1521.
- Wilson, M. A. (2002). The practice of natural family planning versus the use of artifical birth control: Family, sexual and moral issues. Catholic Social Science Review, 7, 185–211.
- Zinaman, M., Drobnis, E. Z., Morales, P., Brazil, C., Kiel, M., Cross, N. L., Hanson, F. W., & Overstreet, J. W. (1989). The physiology of sperm recovered from the human cervix: Acrosomal status and response to inducers of the acrosome reaction. Biology of Reproduction, 41(5), 790–797.





