Health Behavior Change: How to Better Understand Your Patients
As part of its mission to change how health is prescribed and help people get better, Fullscript developed the Treatment Adherence in Integrative Medicine report in 2021. In that report, Fullscript identified behavioral factors and interventions as key contributors to treatment adherence. Thus, the Behavioral Change (BC) Project was initiated to delve further into these factors to better support practitioners and their patients in changing and maintaining healthy behaviors.
Similar to Fullscript’s treatment adherence report, Fullscript’s Medical Advisory Team has now produced a BC white paper. It is composed of a literature review and a patient survey, and focuses on the context of integrative medicine. The project sought to develop key recommendations, tools, and other resources for integrative practitioners looking to support their patients’ behavioral change journeys.
This article provides a high-level summary of the BC project’s main findings, but readers are encouraged to refer to the white paper for greater context and more information.
Defining behavioral change
Behavioral change can be defined by the reshaping of a person’s (health) behaviors. (1)(60) In the context of health promotion and medicine, BC typically implies some kind of sustained benefit to the well-being of the individual without further practitioner support. (53)
The Transtheoretical Model of Change below outlines that BC is made up of six stages:
- Pre-contemplation: The individual is (un)aware of a problematic or beneficial health behavior or is not yet considering change.
- Contemplation: The individual is considering change.
- Preparation (determination): The individual is planning to make change.
- Action: the individual initiates change by stopping a harmful behavior or starting a beneficial one, usually within six months.
- Maintenance: The behavior is continuously performed, usually past six months.
- Relapse/termination: The individual regresses back into any one of the prior stages or stops efforts to continue the behavior at any point in time (or not at all). (59)

Steps to supporting patients’ behavioral change journeys
You can follow five steps to better delivery behavioral change techniques (BCTs) and support their patients’ health journeys. (3)(45)(46)(58)

Step 1: Build awareness
Making yourself and your patients more aware of the importance of healthy behavioral and lifestyle changes is crucial to improving health outcomes.
The inability to change behavior or lifestyle habits is one of the top reasons why patients are unable to follow treatment recommendations long-term. When prolonged, unhealthy lifestyle and behavioral factors contribute to increasing chronic disease rates, (9)(38) which in turn may lead to 90% of the yearly spend ($4.1 trillion) on healthcare (10) and to 40 to 50% of deaths in the United States. (44)(49)
Conversely, adopting healthy behaviors can reduce high mortality rates.

Adopting multiple behaviors is associated with reductions in the risk of all-cause mortality. (39)
Therefore, if practitioners learn to better support behavioral and lifestyle changes, patients will be more likely to achieve better health outcomes and be more satisfied with their care. The country will also experience reductions in chronic disease rates and the associated healthcare costs.
However, providing BC support can be challenging.

There are challenges associated with delivering behavioral change support in the current mainstream medical model. (28)(34)(35)(36)
Fortunately, integrative medicine is well poised to support behavioral and lifestyle changes because it has a foundation in lifestyle medicine (73) and can intrinsically help with motivation and patient engagement.
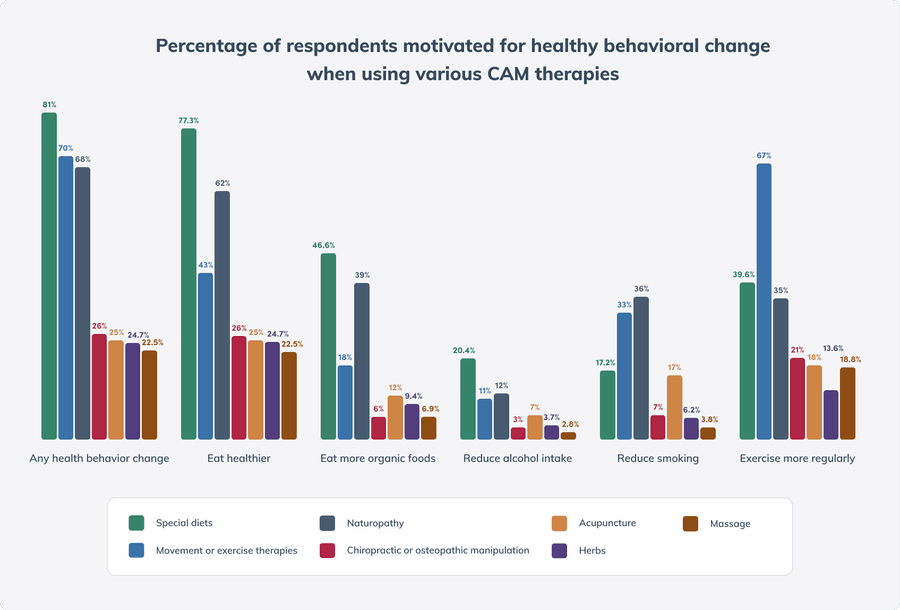
Patients engaging in complementary and alternative treatments often report feeling motivated to engage in other healthy behaviors. (7)
Did you know? Using supplements motivated 16% of adults to exercise more frequently, 22% to eat healthier, 4.6% to reduce alcohol intake, and 5.6% to reduce smoking. (67)
Nonetheless, patients receiving integrative care can still require support from their practitioners, especially if they feel that some aspects of their treatment plan are harder to follow than others.
Did you know? 93% of Fullscript patients believed that at least some change was needed to improve their health. Physical activity, mindfulness, nutrition, and sleep recommendations were perceived to be harder to follow than using supplements, lab testing, and pharmaceuticals.
Ready to start delivering better patient care?
Join 100,000 healthcare providers who rely on Fullscript to dispense top-quality supplements and labs to their patients.
Step 2: Assess
Using a number of techniques to assess your patient’s individual behavioral change needs is critical to personalizing their path to wellness and improving the likelihood of treatment adherence.
Using open-ended questions from motivational interviewing (MI) techniques can be useful in eliciting what needs to occur to best support a patient with BC. (47)(48) Examples of open-ended questions you could ask include:
- How can I help you with…?
- Can you help me understand…?
- How are you feeling about…?
- What are your options?
- Tell me about your goals with…?
- What do you want to do next?
Evidence supports the behavioral change benefits of MI in multiple behaviors, including:
- Alcohol, smoking, and substance abuse (23)
- Dietary intake (65)
- Medication adherence (4)
- Physical activity (6)(52)
- Screening (11)
- Self-management of conditions (13)(18)(25)(43)(64)
- Weight management (24)(68)
For an official directory for MI resources and training, please refer to the MINT website.
Using validated tools that ask questions related to BC can also be helpful for you to understand what needs to happen to best support BC. Examples are found in the table below. Several other validated tools measuring self-control, impulsivity, cognitive flexibility, threat perception, self-affirmation, self-identity, and more (51) can be found in The National Institutes of Health (NIH)’s Science of Behavior Change database.

The use of valid and reliable questionnaires to measure readiness to change or patient empowerment can be helpful to understand your patient’s needs. University of Rhode Island Change Assessment Scale (URICA) (17)(41); Health empowerment Scale (HES) (5).
Step 3: Facilitate empowerment
Empowerment involves ensuring that both you and your patients both have the necessary information and tools at your disposal to support healthy behavioral changes.
Uncover the underlying barriers and reasons your patients may be having challenges with BC. The uptake and maintenance of healthy behaviors can be influenced by many factors including:
- Environmental restrictions (e.g., distance, location, safety)
- Financial cost
- Firmly established attitudes and behaviors
- Lack of access (e.g., transport, facilities, resources)
- Lack of knowledge
- Lack of time (e.g., due to life responsibilities)
- Low socioeconomic status (33)
The top BC barriers for Fullscript patients were:
1. Cost of treatment/appointments
2. Time
3. Motivation, attitudes, and beliefs
Research now focuses on identifying the specific techniques that most effectively improve BC specific to the patient’s underlying needs or barriers. An interactive tool to identify appropriate techniques based on a patient’s given needs can be found here. (8)(30)
For example, providing instructions (a BC technique) might be helpful for a patient who lacks knowledge (the underlying mechanism of action), but might not be as helpful if they lack motivation. Rather, goal setting (a BC technique) would be more effective to boost motivation (the underlying mechanism of action) and would be more likely to lead to BC.

Step 4: Provide strategies
Based on your assessment and the directions of your empowerment focus, the strategies that you deliver should now be tailored to your patients needs.
Did you know? Fullscript patients felt that the most useful strategies were:
1. Receiving education or treatment plan simplification
2. Creating goals, action plans, and making commitments
3. Practitioner monitoring and feedback
There are a number of broadly applicable strategies that are relatively reliable for improving the likelihood of behavioral change across contexts. In a 2010 synthesis of 62 meta-analyses, BC interventions were shown to produce small effects on improving behaviors (d= 0.21). (29) However, even small effects can translate into meaningful outcomes. Examples of such techniques are provided below.

Step 5: Utilize technology
Whereas traditional BC interventions have been mainly conducted face-to-face, which allows for observation of a patient’s physical cues and the benefits of in-person social dynamics, technological interventions may provide other benefits. These benefits include accessibility, cost efficiency, and elimination of barriers that prevent patients from disengaging as a result of the need to be physically present for a consultation or intervention. (2)
Did you know? Most of Fullscript’s patients (82%) would consider using technology to support their BC wellness journeys.
The table below provides a summary of effects found across various digital health interventions. For a full list of evidence, please refer to the white paper.

There is strong evidence to support the use of technologies to help with changing a variety of health behaviors.
One of the most important predictors of a patient’s willingness to adopt and use technology to support their BC journeys (and thus, its efficacy) is the extent to which the digital platform can engage the patient in its supportive interventions. (21)(40)(70)(75)
If opting to use technology to support BC, use the following list to identify specific features and factors that improve patient uptake and engagement:
- Available user guidance
- Embedded practitioner support
- Features to reduce cognitive load
- Goal setting
- Low-cost
- Patient app literacy skills
- Patient awareness of the app
- Perceived utility of the app
- Personalization
- Positive feedback
- Positive tone
- Health information availability
- Reminders
- Stats on progress
- Rewards
- Self-monitoring functionality
- Social support/networking (19)(63)(69)
To reiterate, the use of technologies that are helpful for engaging patients long-term is key. Fullscript patients tended to indicate that the longer they were working with their practitioners, the more likely they were to consider themselves as “acting” or “maintaining” their desired behavioral changes.

The bottom line
Through the steps of building awareness, assessing, facilitating empowerment, providing strategies, and utilizing technology, you can be better equipped to support long-term change and improved health outcomes for your patients. These steps may be particularly important for those patients who require added support in changing and maintaining healthy behaviors.
Ready to start delivering better patient care?
Join 100,000 healthcare providers who rely on Fullscript to dispense top-quality supplements and labs to their patients.

